Browse through our Journals...
An Unusual Cause Of Mediastinal
Lymphadenopathy
First and corresponding author: SG Chong,
Respiratory Registrar, Mid-Western Regional Hospital,
Limerick, Dooradoyle, Limerick, Ireland.
Second author: A O’Brien, Consultant Respiratory
Physician, Mid-Western Regional Hospital, Dooradoyle,
Limerick, Ireland.
Third author: BP Casserly, Consultant Respiratory
Physician, Mid-Western Regional Hospital, Dooradoyle,
Limerick, Ireland.
Key words: phenytoin, mediastinal lymphadenopathy, hilar lymphadenopathy,
lymphoma
Abstract
Phenytoin-induced lymphadenopathy was first described in 1940 by Coope and Burrows.
Since then, there had been various case reports concerning phenytoin manifestations. We report a case of a 40 year old woman who presented with bilateral hilar and mediastinal lymphadenopathy 8 years after taking phenytoin. Biopsy showed normal lymphoid tissue with no evidence of granulomas. The hilar and mediastinal lymphadenopathy resolved 2 months after cessation of phenytoin.
Case Report
We report a case of a 40 year old woman who presented to our respiratory clinic
for assessment of an abnormal chest X-ray (CXR) which demonstrated bilateral hilar and mediastinal lymphadenopathy. The CXR was performed after she complained of
generalised arthralgias for four weeks. The arthralgias involved both shoulders, arms,
wrists, knees and ankles. She also revealed that she was short of breath after walking for 10-15 minutes. Her background history included epilepsy, depression, osteoarthritis and migraine. Her medications were flurazepam, venlafaxine, clonazepam, phenytoin, and levetiracetam. She had been seizure free for the prior 8 years. She was a lifelong nonsmoker.
Figure 1
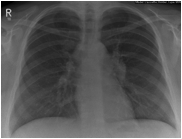
CXR showed bilateral hilar and mediastinal lymphadenopathy.
Figure 2

CT Thorax showed extensive mediastinal lymphadenopathy.
Examination revealed a heart rate of 72 beats per minute, BP 116/75 mmHg and
SpO2 96% on room air. Chest auscultation was clear with normal heart sounds. There was some bruising noted on both legs. The presumptive diagnosis at that point was
sarcoidosis.
Bloods were normal including serum calcium. Serum ACE level was 47 (give
units and normal range). X-ray of both knees showed osteoarthritic changes.
CT thorax showed extensive mediastinal lymphadenopathy. Her case was
discussed at the weekly multi-disciplinary radiology meeting. The consensus was that she had sarcoidosis radiologically. Bronchoscopy with transbronchial biopsy was performed.
No endobronchial lesions were seen. Biopsy demonstrated normal tissue cells with no
evidence of granulomatous inflammation. As she was seizure free for the last 8 years, the phenytoin was stopped. Two months later, she had repeat CXR which showed
improvement of the hilar adenopathy. This was confirmed by CT thorax which showed
complete resolution of the mediastinal lymphadenopathy.
Discussion
Phenytoin use has been associated with various lymph node abnormalities. Four
distinct categories of lymphadenopathy have been described: lymphoid hyperplasia,
pseudolymphoma, pseudo-pseudolymphoma and lymphoma1. Lymphadenopathy in
association with the use of hydantoin derivatives such as phenytoin was first described in 1940 by Coope and Burrows2. In 1959, Saltzstein and Ackerman3 reviewed 75 cases and reported a further seven patients, two of whom subsequently died 5 years later due to lymphoma. In 1966 Hyman and Somers4 reported 6 patients on anticonvulsant therapy who developed a histologically proven Hodgkin’s lymphoma or lymphosarcoma. Games5 et al. reported a case in which phenytoin induced lymphadenopathy regressed after cessation of therapy.
More recent publications divide these occurrences into two; the anticonvulsant
hypersensitivity syndrome, and the phenytoin-induced pseudolymphoma6. The
anticonvulsant hypersensitivity syndrome generally develops within eight weeks after the drug is first prescribed6. The presenting symptoms are fever and malaise in most
patients6.
In contrast to the hypersensitivity syndrome, phenytoin-induced pseudolymphoma
is considered to be a late effect of phenytoin therapy, which can occur years after
initiating treatment, as in our case study6.
Evaluation of patients who develop enlarged lymph nodes while receiving
phenytoin therapy should be done carefully so that phenytoin-induced lymphadenopathy
may be differentiated from true malignant lymphoma and appropriate treatment may be
given7. John et al6 describe a case of phenytoin-induced pseudolymphoma in which the
flow cytometry analysis of peripheral blood and bone marrow mononuclear cells detected identical T cell population with an aberrant immunophenotype6. In addition to that, a T cell receptor beta gene was found to be clonally rearranged in both peripheral blood and bone marrow, supporting a clonal origin of atypical T cells6. However, this clonal population of T-cells could not be detected in a pathologic specimen obtained from excisional biopsy of patient’s cervical lymph nodes6. After discontinuing the patient’s phenytoin, lymphadenopathy had nearly completely resolved and the circulation clonal T cell population had disappeared at re-evaluation 12 months later.
Harris et al1 recommended the use of the analysis of immunoglobulin and T cell
receptor genes in establishing the lineage and clonality of lymphoproliferative disorders
in the assessment of dermatopathic lymphadenopathy
The mechanisms underlying the development of lymphadenopathy in patients
treated with phenytoin are not completely understood6. With regards to the anticonvulsant hypersensitivity syndrome, it has been proposed that abnormal detoxification of reactive metabolites of phenytoin, possibly arene oxide metabolites produced by cytochrome P450, is responsible for the syndrome6.
Cessation of phenytoin have been documented to resolve the lymphadenopathy.
Steroids may be helpful in cases of resistant lymphadenopathy.
On conclusion, the pathophysiology of phenytoin-induced lymphadenopathy is
incompletely understood. It can require careful pathological scrutiny to differentiate it
from monoclonal cell expansion. Given the number of patients regularly using phenytoin, it is an important clinical entity that general physicians need to be cognisant of.
References
1. Harris DWS, Ostlere L, Buckley C, et al. Phenytoin-induced pseudolymphoma. A report of a case and review of the literature.Br J Dermatol1992;127:403-406.
2..Coope R. Burrows RGR. Treatment of epilepsy with sodium diphenylhydantoinate.Lance 1940; i 490-2.
3. Saltzstein SL, Ackerman LV. Lymphadenopathy induced by anticonvulsant drugs and
mimicking clinically and pathologically malignant lymphomas. Cancer 1959; 12;164-82
4..Hyman GA, Sommers SC, the development of Hodgkin’s disease and lymphoma
during anticonvulsant therapy. Blood 1966; 28; 416-27.
5. Gams RA, Neal JA, Conrad FG. Hydantoin-induced pseudo-pseudolymphoma. Ann
Intern Med 1968; 69: 557-68.
6. Johns ME, Moscinski LC, Sokol L. Mediterr J Hematol Infect Dis. 2010 Sep
7;2(2):e2010028.
7. Schwinghammer TL; Howrie DL, Drug Intelligence & Clinical Pharmacy 1983 Jun;
Vol 17 (6), pp. 460-2.
Copyright Priory Lodge Education Limited 2012 -
First Published January 2012
Click
on these links to visit our Journals:
Psychiatry
On-Line
Dentistry On-Line | Vet
On-Line | Chest Medicine
On-Line
GP
On-Line | Pharmacy
On-Line | Anaesthesia
On-Line | Medicine
On-Line
Family Medical
Practice On-Line
Home • Journals • Search • Rules for Authors • Submit a Paper • Sponsor us
All pages in this site copyright ©Priory Lodge Education Ltd 1994-


