 TUBERCULOSIS: no longer down and out
TUBERCULOSIS: no longer down and out
P D O Davies, MA DM FRCP, Director,
Tuberculosis Research Unit, Cardiothoracic Centre,
Thomas Drive, Liverpool, L14 3PE, UK
First Published December 1996
Cases of Tuberculosis in England and Wales increased from 5,086 in 1987 to 5,961 in 1993: a 17% increase. Some notorious hot spots such as Leicester and Bradford actually showed a decrease of about 15% over these 6 years, but others such as Leeds (11%), Manchester (12%) and inner London (25%) showed substantial increases. But top of the bill with a (30%) increase came Liverpool.
One of the reasons for this is lack of awareness of the problem, not just from the public but from the family doctor. One of my recent patients, a white Liverpudlian man of 57 told an interesting story. He had had tuberculosis of the abdomen as a 12 year old child. He had been treated and got over it. He had lead an active working life, well, fit, bit of smoker, but otherwise no vices. Then about a year before he saw me he began to feel unwell. His semi-chronic smokers cough became harsher and more persistent. He began to lose weight, a loss that amounted to nearly 3 stone by the time he saw me. He developed chills and sweating especially at night. He went to see his family doctor many times in the course of his illness and even told him that he might have TB and asked 'shouldn’t I have a chest x-ray?' "Of course not", would come the reply, " nobody in Liverpool gets TB these days".
The way he came to me was even more worrying. His ten year old grandson became unwell and pulmonary tuberculosis was diagnosed at the Children’s Hospital (Fig1).
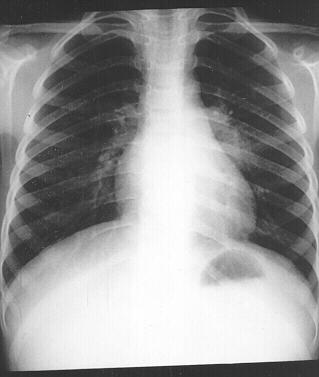 |
| Figure 1 Ten year old boy with tuberculosis |
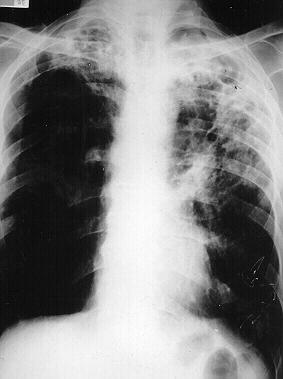
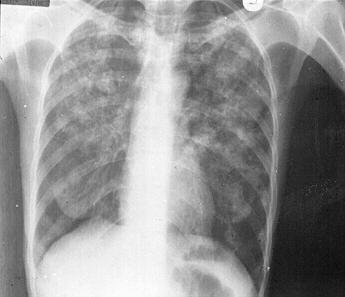
Contact tracing reacted smartly and three days later Mr Madden (not his real name) was marched into my contact clinic, where we took his chest x-ray (Fig.2) and all was revealed: extensive cavitating tuberculosis which turned out to be heavily smear positive.
 |
| Figure 2 Extensive cavitating tuberculosis |
Mind you it’s a bit unfair to blame the family doctor, when only 4 years ago Mrs Bottomley, the then UK Health Minister said that "Tuberculosis has been virtually eliminated." That statement alone was probably worth an increase of 5% in case numbers as family doctors all over the country breathed a sigh of relief and failed to diagnose the next three cases which came their way, confident in the ministerial reassurance that TB was well and truly defeated.
Fortunately we found no further cases among Mr Madden’s family and friends, but his close contacts will remain under review for a full six months. Mr Madden himself refused to come into hospital initially so I started him on the "Best Buy" treatment of Isoniazid, Rifampicin and Pyrazinomide in the single formulation tablet called Rifater (Hoechst Marrion Rousell). Within a week of starting the treatment he coughed up a whole lot of blood and scampered into hospital pretty quick.
Fortunately it all settled down on medical treatment and we were able to send him home. Profuse haemoptysis is one of the commonest causes of death from extensive pulmonary tuberculosis and the thoracic surgeons are never dreadfully keen in performing emergency lobectomies in the middle of the night on patients who are heavily sputum smear positive. Neither are pathologists come to think of it and they only work during the daylight hours.
I saw Mr Madden for his two month follow-up appointment recently. He is doing well and has put on two stone in weight. His chest x-ray is improving and the cavity at the left apex is shrinking nicely. More good news: sensitivity results showed the bugs to be fully sensitive so I was able to reduce the regimen to Isoniazid and Rifampicin alone, again using a combination product (Rifinah) which prevents accidental drug resistance developing as a result of the patient taking only one instead of two or three compounds.
It was a few years ago (July 1992) that my juniors proudly presented me with three chest x-rays as I started my ward round one Monday morning. The first was of a man of 69 who had had tuberculosis 15 years previously. He had remained fit following this until his present illness. He had complained of a chronic productive cough, with sputum occasionally flecked with blood, for three to 4 months. (Fig.3) During that time he had lost over a stone in weight and suffered from sweats and fevers.
 |
| Figure 3 Man of 69 with past history of tuberculosis |
The second X Ray was of his 43 year old son with an identical history and as you can see virtually identical chest x-ray (Fig.4).
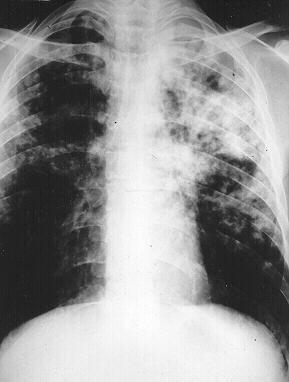 |
| Figure 4 43 year old male |
Both men were sputum smear positive and were admitted to the medical ward for an initial period of observation while treatment was started. The third x-ray was of the 18 month old son of the son. He had been asymptomatic but when the disease in his father and grandfather had been discovered, contact tracing had been swift and after a ragingly positive mantoux test he had been x-rayed and the characteristic middle lobe collapse of primary tuberculosis found (Figure 5).
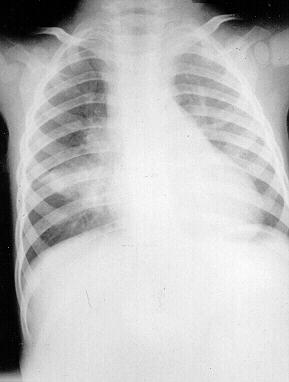 |
| Figure 5 18 month old male |
He had been admitted to the Children’s Hospital. The grandmother developed a patch on the three month follow-up chest x-ray at the contact clinic .
Over the next three months two other patients with tuberculosis, apparently with no contact with each other were admitted, treatment started and discharged. By serendipidity both were recalled to follow-up clinic on the same day and recognised each other from a social club they frequented. Further chat revealed that they had the same disease. A little further probing from the patients also revealed that the club was frequented by the grandfather mentioned above. Waiting more than half an hour for your appointment can have its advantages.
Contact tracing did a further trawl on barmen in the club and found a further two cases. The trawl was extended to the three hundred club members but no further cases were found. Unfortunately one member who failed to attend for screening presented with tuberculosis meningitis over a year later, but disease was so severe that he died soon after treatment was started. Fingerprint analysis of the bug showed it to be the same strain as affected the social club members. Nine cases including one death from an initial index case. If the family doctor had got on to the diagnosis of the index case sooner a lot of trouble could have been avoided.
There is little doubt that tuberculosis is now increasing globally. This country saw a 17% rise in cases between 1987 and 1993 similar to that of the USA. The increase has stopped for the moment but the number of case, (6,248 in 1995 in the UK) remains stubbornly high. WHO estimates a world-wide increase of up to 40% in the next 20 years. There are a number of reasons for this. The single most important is demographic. This will account for about 75% of the increase. Population growth of 70% in South East Asia and 150% in Sub-Saharan Africa in the next 30 years, the areas of the world where tuberculosis is most prevalent will increase the number of cases dramatically. HIV is implicated in certain areas but its impact is only just beginning to be felt. Whereas one third of the world’s population, 1.7 billion is estimated to be infected with the tubercle bacillus, only 24 million are estimated to be HIV positive. But in the individual who is dually infected with HIV and TB the risk of developing the disease rises from 10% in a life-time to 10% in a year. This is why case rates in Malawi and South Africa have increased by as much as ten fold in a decade.
Coinfection with tuberculosis and HIV in the UK is low, mainly because the two infections tend to be present in different risk groups but about 5% of HIV case have tuberculosis and about 2% of tuberculosis cases in the UK are HIV positive. Disease in the HIV positive patient case be harder to spot . The chest x-ray (Fig6.) tends to show widespread shadowing, cavitation is less frequent so that smear positivity is less common making the diagnosis harder to confirm.
 |
| Figure 6 HIV positive patient with Tuberculosis |
Non respiratory sites such as the lymph glands tend to be commoner (Fig.7). Provided treatment is started promptly HIV positive disease apparently responds as well as HIV negative.
 |
| Figure 7 Lymph Gland TB |
Migration probably accounts for most of the increase in developed countries including our own. In 1993 56% of notifications of tuberculosis were in ethnic minorities, of which Africans showed the steepest increase.
Since the 1960s we have been aware that tuberculosis is 20 to 30 times commoner in South Asians than in the white population. Non-respiratory sites of disease are up to 100 times commoner in this group in the UK. In decreasing order of frequency, there are, lymph nodes, usually cervical bone and join of which spinal disease accounts for half, abdominal abscesses at virtually any site, genito-urinary, menigeal and miliary. Unless the diagnosis of tuberculosis is considered in these cases, appropriate specimens, such as biopsy for smear and culture, may not be collected and the diagnosis missed.
Poverty is back on the agenda. Publications from Liverpool and London shows the strong association between poverty and TB remains, and as poverty increases so does TB. Amongst the homeless in London case rates are higher than in HIV affected sub-Saharan Africa (2% of vagrants had active TB in one study. Lack of awareness that TB is still a problem, as illustrated by the cases, is certainly contributing to the increase. A Stitch in time saving 9 would be an appropriate motto for anyone interested in tuberculosis control. The until now, complacent health policy decision making has resulted in tremendous loss of expertise and resources in fighting the disease.
Longevity too is playing a part in the increase. In developed countries, the highest rates are in the elderly, because they are the ones who were infected in early life as they lived through times of high prevalence. With ageing comes a decline in immunity and reactivated disease in those harbouring remote infection. As life expectancy improves in developing countries this trend may increase.
Finally the dreaded prospect of drug resistant disease is raising its ugly head. The first line drugs we have for the treatment of tuberculosis are Isoniazid, Rifampicin, Pyrazinamide and Ethambutol. Resistance to the first two whether or not there is resistance to other drugs, is commonly defined as "mult-drug resistance". It is this form of resistance which is so worrying. Without Isoniazid, the most rapid killer of the TB bug, patients may remains sputum smear positive and therefore infectious for months into their treatment instead of becoming non-infectious by two weeks. Without Rifampicin, the best killer of the slowly dividing persistent bugs, treatment length increases to 18 months or more to prevent replapse.
The potential of drug resistant tuberculosis is now very real even in the UK which probably has the lowest incidences of drug resistance in the world. For example I had a patient recently who had been treated for tuberculosis in a developing country and had relapsed with sputum smear positive disease I needed to know the drugs she had been taking previously. They were the "top four": Isoniazid, Rifampicin, Pyrazinamide and Ethambutol. To be on the safe side I had to assume that she might have a bug resistant to all these. However, because Isoniazid and Rifapicin are so important in the treatment and keeping it to as little as six months, she had to have these until the sensitivity results came through. Therefore I had to give her these two plus another three which she had never had before. I picked Streptomycin, Prothionamide and Ciprofloxacin and held my breath unto sensitivity results came through. I treated my micobiological colleagues to a round at the bar and asked them very politely how soon they would get the results. In the end they did OK 28 days from sputum reception to sensitivity results. Not bad but we will have to get quicker with expensive molecular techniques if we are going to beat the multiply drug resistant bugs.
She turned out to have resistance to Isoniazid and Streptomycin. That was almost bad luck. She had never had Streptomycin so the only way she could be resistant to is was by acquiring a streptomycin resistant bug for her first infection. The Isoniazid resistance probably developed during treatment of her first attack due to haphazard drug taking, which is probably why she relapsed as well. Had she also been resistant to Rifampicin she would effectively had been on only two weak second line drugs for a month before we knew what were treating. Such is the way that drug resistance can breed more drug resistance.
The UK Government has begun to respond to the renewed threat of tuberculosis. The report I am waiting for is its contribution to the control of tuberculosis internationally. Just as no man is an island sufficient of himself, so no island is an island in infectious terms. The protective moat we are ringed with, "against infection and the hand of war" so eloquently described by John of Gaunt in Richard II, offers no defence against tuberculosis. We must play our part in an international strategy to eliminate this killer.
In the meantime every medical worker should be aware that the next patient may have tuberculosis.
Home • Journals • Search • Rules for Authors • Submit a Paper • Sponsor us
All pages copyright ©Priory Lodge Education Ltd 1994-

