Browse through our Medical Journals...
GLOBAL CLINICAL CHANGE: DIFFERENCES BETWEEN THE PATIENT'S AND THE CLINICIAN'S ASSESSMENT THROUGHOUT THE TREATMENT OF A DEPRESSIVE EPISODE
Antoni Corominas, Ana Adan and Tina Guerrero
Department of Psychiatry, Hospital General Manresa (Barcelona), Universitat de Barcelona, and Pharma Consult Services
Corresponding author: Antoni Corominas, MD Department of Psychiatry, Hospital General de Manresa La Culla s/n 08240 Manresa (Barcelona) SPAIN e-mail: corominas@sumi.es
Abstract
Background Results from previous research show small concordance between the patient's and the clinician's assessment. Some studies with depressive patients have shown that the correlation between self-assessment and clinician's assessment was weaker at baseline than at discharge. This study aims to evaluate the agreement between self-assessment and assessment by the clinician of the global clinical change throughout the treatment of a depressive episode. Methods In a drug surveillance study of the antidepressant citalopram, the scores of patients' and clinicians' assessment of global change (Global Clinical Impression Scale) were compared, grouping those patients that showed any kind of improvement in each follow-up assessment (after 4, 8 and 24 weeks of treatment). Results N=1.138. Follow-up at 4 weeks: improvement according to the clinician's assessment = 80,7 %; improvement (patients self-assessment) = 73,1 % (p<0,0001, Chi-square. Follow-up at 8 weeks: 95% of the patients improved (clinician's assessment) and 92.5% improved according to the patients self assessment p<0,0001. Follow-up at 24 weeks: improvement in 95.9% (clinician's assessment) and 94.9% (patient's assessment), p<0,0075. Conclusions There are differences between the patient's and the clinician's assessment, especially when a complete remission of the depressive symptoms has not yet appeared in a considerable percentage of patients (after the first month of treatment). This could be partly explained by the bias of a worse self-assessment until the depressive episode has been controlled.
Introduction
The better understanding of the relations between the subjective assessment of the course of the illness, or the change experienced with the treatment and the clinician evaluation has important implications from a clinical perspective. If the information regarding the agreement of both assessments is not taken into account, mistakes or inaccuracies may emerge from the evaluation of therapeutic results. Some studies with depressive patients have found that the correlation between self-assessment (BDI, Beck Depression Inventory; Beck et al, 1961) and clinician's assessment (Hamilton Rating Scale for Depression; Hamilton, 1967) were weaker at baseline than when the patient was discharged (Bailey and Coppen, 1976; Martinsen et al, 1995). The lack of insight of these patients and their pessimistic view might lead them to poorer evaluations, resulting in a low reliability of the exclusively subjective assessment (Bobes, 1997). However, as it is shown by some studies about quality of life (Wells et al, 1989; Hays and Wells, 1995), this same bias seems to exist in patients with serious illnesses.
Kwoh et al (1992) point out that the clinicians and their patients with rheumatoid arthritis often disagree in their assessment of the degree of physical and mental impairment that the patient experiences. In their study, the weighted kappa statistic was 0.39 for physical functioning and 0.30 for mental functioning. Nowadays, there are not precise enough parameters regarding the suitability of self-assessment in the several psychiatric disorders, in the different stages of the follow-up, or with regard to the clinician's assessment. This study aims to examine the differences between self-assessment and clinician's assessment throughout the treatment of a depressive episode. Specifically, the clinician's and the patient's assessments were compared, regarding the global change experienced throughout every stage of follow-up, with a total of 3 assessments in a 6-month treatment period.
Method
In a multicentric, prospective, observational and open-label drug surveillance study of the antidepressant drug citalopram (Menchón et al, 1997; Corominas et al, 1998 (a, b), the scores on the Clinical Global Impression - Change Scale (CGI; Guy, 1976) were recorded. This is an observational scale of global evaluation, which assesses the change in degree of illness in relation to the original assessment. It can be applied to any type of patients, regardless of the diagnosis. The scale has only one item that measures global change of the illness (improvement or worsening) by the clinician and by the patient, separately, on a 7 point scale from 0 to 6, becoming a valid, reliable and widely used instrument (Bech et al, 1993).
Subjects were 1138 patients with major depression according to ICD-10 criteria who completed a follow-up period of 24 weeks. All were aged over 50, so it was intended to focus the study on patients with higher comorbidity and consumption of other drugs. Patients were included in the study consecutively by the psychiatrists, assigning treatment with citalopram (adjusting the doses openly and individually according to the clinical response and the side effects). The patients were interviewed again after 4, 8 and 24 weeks (independently of the follow-up visits that each psychiatrist considered appropriate). The scores on the CGI-Change (patient's and clinician's assessment), the Montgomery-Asberg Depression Scale (Montgomery and Asberg, 1979) and the UKU's Side Effect Scale (Lingjaerde et al,1987) were recorded at each interview.
Statistical analysis Descriptive analysis of the baseline characteristics of the sample, according to the demographic and clinical variables, and the scores in the above-mentioned scales, using absolute and relative frequencies and central tendency and dispersion measures were performed. To examine the differences between the clinician and the patient in the assessment of change, we grouped the patients that experienced an improvement (scores 1, 2 or 3, that stand for "very much improved", "much improved" and "minimally improved", respectively) in each of the follow-up interviews according to the clinician's and the patient's assessment, after 4, 8, and 24 weeks of treatment. The statistical analysis of the nominal values of this new variable (clinical improvement versus no clinical improvement) was carried out with the Chi-square test.
Results
A sample of 1,138 patients that completed a 6-month follow-up while being treated with citalopram was studied. Main social, demographic and clinical characteristics of the patients are shown in table 1.
TABLE 1.
Demographic and clinical characteristics of the sample
(N= 1138 patients)
mean SD Min. Max.
______________________________________________
Age 56.19 12.82 18 91
Gender n %
_____________________________
Male 369 32.4
Female 769 67.6
Type of depressive episode
( ICD-10 criteria; World Health Organisation, 1992)
n %
_________________________________
Single episode 605 53.2
Recurrent 533 46.8
Severity of depressive episode
( ICD-10 criteria; World Health Organisation, 1992)
n %
____________________________
Mild/Moderate 487 42.8
Severe 651 57.2
Scores on Montgomery-Åsberg depression scale
(Montgomery and Åsberg, 1979)
mean SD Min. Max.
_______________________________________________________________
Baseline 30.68 7.9 5 60
1 month 20.65 9.22 0 47
2 months 13 8.62 0 48
6 months 7.92 7.14 0 46
The distribution of the percentages for each of the 7 points of the Clinical Global Impression - Change scale, throughout the successive follow-up visits, and according to assessments made by patients and by clinicians, is shown in table 2.
TABLE 2.
CGI-Change scale
1 month |
2 months |
6 months |
||||
clinician % |
patient % |
clinician % |
patient % |
clinician % |
patient % |
|
| Very much improved | 9.1 |
9.5 |
34.1 |
32.6 |
64.3 |
60 |
| Much improved | 25.7 |
23.7 |
37.6 |
31.3 |
22.9 |
24.2 |
| Minimally improved | 45.9 |
39.9 |
23.3 |
28.6 |
8.7 |
10.7 |
| No change | 17.8 |
23.1 |
3.8 |
5.6 |
2.4 |
3.2 |
| Minimally worse | 1.1 |
2.8 |
0.6 |
1.1 |
0.7 |
0.8 |
| Much worse | 0 |
0.4 |
0.2 |
0.3 |
0.4 |
0.4 |
| Very much worse | 0.1 |
0.3 |
0.1 |
0 |
0.1 |
0.2 |
| Not evaluated | 0.4 |
0.4 |
0.4 |
0.4 |
0.5 |
0.5 |
Grouping the patients that experienced an improvement in each of the interviews, as described under "Methods", two facts can be observed (figure 1): - A progressive increase of patients showing an improvement, even though after one month of treatment this proportion is already very high. Percentage of patients showing an improvement is even higher at two months, while minimal differences can be observed between second and third months. - Assessments made by clinicians and patients showed some differences, particularly at first follow-up.
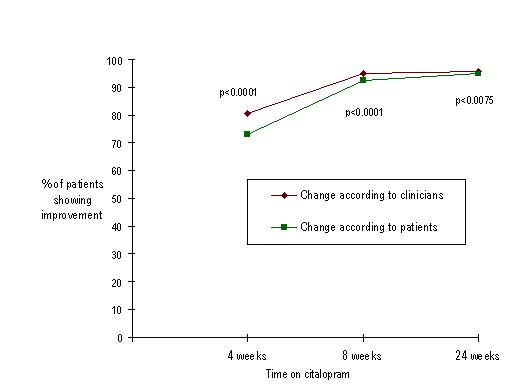
Patient's perceptions of improvement tended to be lower than assessments made by clinicians, although this difference tended to decline with time when treatment was continued. At follow-up 1, 80.7 % of patients had improved (according to clinician's assessment) versus 73.1 % (self-assessment), Chi-square= 475.82, p<0.0001. At follow-up 2, corresponding rates were 95 % (clinician's assessment) and 92.5 % (patient's assessment), Chi-square= 212.89, p<0.0001. At follow-up 3, improvements were 95.9 % (according to clinician's assessment) and 94.9 % (patient's assessment), Chi-square= 83.13, p<0.01.
Discussion
Both the type of instrument and who is going to perform the assessments are key aspects when examining clinical change or improvement. The validity of the studies that aim to test the effectiveness or the results of a specific treatment may be questioned if the assessment is based only on one source or if the concordance between instruments and assessing subjects is not taken into account. This study shows that assessments made by patients and by clinicians show some differences, particularly when a definite improvement of depressive symptoms has not yet appeared in a substantial number of patients (after one month of treatment). This finding suggests that the differences are largely due to the bias of a more negative self-assessment until the depressive episode has been controlled. The findings of previous research suggest that there is small congruence between measures coming from different rating sources, both in relation to the instrument as well as the assessing subject. Thus, a poor concordance has been found between the patient's self-assessment and the clinician's assessment (Clark and Friedman, 1983; Bell et al, 1986; Conte et al, 1988; Sullivan and Grubea, 1991). Piersma et al (1995) did not find significant relationships between symptom distress reported by patients (according to the Brief Symptom Inventory) and global functioning rated by clinicians (according to the Global Assessment of Functioning Scale). If we specifically consider the evaluation of clinical change, Fischer et al (1996) showed that the traditional instruments used to measure the clinical change in rheumatoid arthritis (comparison throughout time of the scores in pain and disability scales) scarcely correlated with the perception of change by the patient. In addition, the patient's satisfaction was directly related to his perception of clinical change, and not with the standardised measures assessed by the clinician. Moreover, patient perception of change was also shown to be at least as sensitive to change as the traditional measures. The results of our study are perhaps more consistent since the same scale was used by patients and clinicians alike to assess changes. Thus, even under these conditions, it seems that monitoring the clinical response should not rely on one only subject's evaluation or one only instrument. We would also like to highlight that the differences between patients' ratings and clinicians' ratings tended to disappear when treatment was continued, in parallel with the improvement of depressive episodes in most patients completing follow-up. This suggests the need to a longitudinal approach in the evaluation of the insight, self-assessment and clinical change in psychiatric disorders.
References
Bailey, J. & Coppen, A. (1976). A comparison between the Hamilton Rating Scale and the Beck Inventory in the measurement of depression. British Journal of Psychiatry 128, 486-89.
Bech, P., Malt, U.F., Dencker, S.J., Ahlfors, U. G., Elgen, K., Lewander, T., Lundell, A., Simpson, G. M. & Lingjaerde, O. (1993). Scales for assessment of diagnosis and severity of mental disorders. Acta Psychiatrica Scandinavica 87, Suppl 372.
Bell, M., Billington, R. & Becker, B. (1986). A scale for the assessment of object relations: Reliability, validity and factorial invariance. Journal of Clinical Psychology 42, 733-741.
Bobes, J., González, M.P., Saiz, P. & Bousoño, M. (1997). Calidad de vida y depresión (Quality of life and depression). In Opinión. Actualidad del trastorno depresivo: Consecuencias sociales de la depresión, 6. Adis International Limited: Madrid.
Clark, A., Friedman, M.J. (1983). Nine standardized scales for evaluating treatment outcome in a mental health clinic. Journal of Clinical Psychology 39, 939-950.
Conte, H.R., Plutchik, R., Picard, S., Karasu, T.B. & Vaccaro, D. (1988). Self-report measures as predictors of psychotherapy outcome. Comprehensive Psychiatry 29, 355-360.
Corominas, A., Menchón, J.M., Adan, A., Segú, J.L. & Guerrero, P.M. (1998 a). Tolerancia y predictores de aparición de reacciones adversas y abandonos en el estudio de farmacovigilancia de citalopram (Tolerability and predictors of adverse reactions and dropouts in the drug surveillance study on citalopram). Actas Luso-Españolas de Neurología, Psiquiatría y Ciencias Afines 26, 155-156.
Corominas, A., Adan, A. & Segú, J.L. (1998 b). Resultados del estudio de farmacovigilancia de citalopram en el tratamiento de episodios depresivos (Results of the drug surveillance on citalopram in depressive episodes). Pharma Consult Services SA, Edipharma:Barcelona.
Fischer, D., Stewart, A., Lorig, K. & Holman, H. (1996). Patient perceptions of clinical change and its meaning correlate poorly with change measured by conventional instruments. AHSR & FHSR Annual Meeting Abstract Book 12, 56-57.
Guy, W. (1976). Early Clinical Drug Evaluation Unit (ECDEU) assessment manual for psychopharmacology. Revised. NIMH publication DHEW publ NO (Adm) 76-338. Bethesda MD: National Institute of Mental Health, 217-22.
Hamilton, M. (1967). Development of a rating scale for primary depressive illness. British Journal of Social & Clinical Psychology 6, 278-296.
Hays, R.D., Wells, K.B., Sherbourne, C.D., Rogers, W.& Spritzer, K. (1995). Functioning and well-being outcomes of patients with depression compared with chronic general medical illnesses. Archives of General Psychiatry 52, 11-19.
Kwoh, C.K., O'Connor, G.T., Regan-Smith, M.G., Olmstead, E.M., Brown, L.A., Burnett, J.B., Hochman, R.F., King, K. & Morgan, G.J. (1992). Concordance between clinician and patient assessment of physical and mental health status. Journal of Rheumatology 19 (7),1031-7.
Lingjaerde, O., Ahlfors, U.G., Bech, P., Dencker, S.J.& Elgen, K. (1987). The UKU side effect rating scale. A new comprehensive rating scale for psychotropic drugs and a cross-sectional study of side effects in neuroleptic-treated patients. Acta Psychiatrica Scandinavica 76 (suppl. 334).
Martinsen, E.W., Friis, S. & Hoffart, A. (1989). A factor analytical study of the Comprehensive Psychopathological Rating Scale among patients with anxiety and depressive disorders. Acta Psychiatrica Scandinavica 80, 492-98.
Menchón, J.M., Corominas, A., Adan, A., Segú, J.L. & Guerrero, T. (1997). Citalopram en el tratamiento de la depresión con patología orgánica concomitante (Citalopram in the treatment of depression comorbid with organic disease). Psiquiatría Biológica 4 (suppl. 2), 87.
Montgomery, S.A. & Åsberg, M. (1979). A new depression scale designed to be sensitive to change. British Journal of Psychiatry 134, 382-9.
Piersma, H.L. & Boes, J.L. (1995). Agreement between patient self-report and clinician rating: concurrence between the BSI and the GAF among psychiatric inpatients. Journal of Clinical Psychology 51 (2), 153-157.
Sullivan, C.W. & Grubea, J.M. (1991). Who does well in a day treatment program? Following patients through 6 months of treatment. International Journal of Partial Hospitalization 7(2), 101-107.
Wells, K.B., Stewart, A., Hays, R.D., Burnam, M.A., Rogers, W., Daniels, M., Berry, S., Greenfield, S. & Ware, J. (1989). The functioning and well-being of depressed patients. Results from the Medical Outcomes Study. Journal of the American Medical Association 262 (7), 914-9.
World Health Organisation. (1992). The ICD-10 Classification of Mental and Behavioural Disorders. WHO: Geneva.
First published August 2nd 2001
Click
on these links to visit our Journals:
Psychiatry
On-Line
Dentistry On-Line | Vet
On-Line | Chest Medicine
On-Line
GP
On-Line | Pharmacy
On-Line | Anaesthesia
On-Line | Medicine
On-Line
Family Medical
Practice On-Line
Home • Journals • Search • Rules for Authors • Submit a Paper • Sponsor us
All pages in this site copyright ©Priory Lodge Education Ltd 1994-


