Browse through our Journals...
Spontaneous Splenic Rupture
Girish H Shivashankar, MRCP (U.K) & James F Kelly, FRCP (U.K)
Erne Hospital, Enniskillen, U.K
Abstract:
Spontaneous rupture of the spleen was first described by the English surgeon, Atkinson, in 1874(1). It is usually associated with infectious, neoplastic, or hematologic diseases. Unlike traumatic splenic rupture, spontaneous rupture of the spleen is not often considered in the differential diagnosis of abdominal pain, can be easily confused with other abdominal pathology & failure to consider splenic rupture can be catastrophic.
We report two such cases of spontaneous splenic rupture. The aetiology proved to be infective endocarditis in one case and ruptured splenic artery anuerysm in the other. The condition was diagnosed and managed immediately which led to favourable outcome in both patients. The cases illustrate the importance of keeping a broad differential in patients presenting with acute abdominal pain and remind the physician to consider the possible diagnosis of spontaneous splenic rupture.
Case 1
A 63 year old lady with past medical history of hypertension and a Transient Ischaemic Episode presented to stroke unit with new onset slurring of speech and right sided deviation of the angle of the mouth. Of importance, on admission she was noted to be pyrexic at 38.7 C with a new heart murmur.
Inflammatory markers and infection count were raised (ESR 55, WCC 11.2 & CRP 71) on admission. Blood cultures were performed. An urgent CT Brain showed multiple tiny infarcts in the left internal capsule in keeping with patient’s symptoms. A presumptive diagnosis of acute bacterial endocarditis was made and IV Benzyl Penicillin & Gentamicin were commenced immediately after advice from the microbiologist.
Trans thoracic Echocardiogram was inconclusive. However, transoesophageal ECHO showed echogenic masses attached to anterior leaflet prolapsing into left atrium with associated moderate to severe mitral regurgitation. Staphylococcus sanguis was isolated from patient’s blood cultures. This organism was sensitive to the prescribed antibiotic regimen. These findings confirmed the diagnosis of Acute Bacterial Endocarditis with associated embolic infarcts and acute stroke illness.
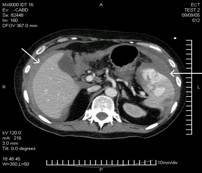
After 3 weeks of treatment with IV antibiotics, the patient was clinically well, and inflammatory markers WCC 9, ESR 32 & CRP 18 had significantly improved. At this stage due to problems with poor peripheral venous access, a central venous access was inserted in the right Internal Jugular vein. Shortly after this procedure patient began to feel weak, went pale and collapsed. Urgent Bloods showed haemoglobin at 5.6 g/dl, a sharp drop from her baseline of 9. Patient was immediately resuscitated, transfused with four units of red cells and transferred to ICU. An urgent CT Abdomen revealed a large amount of blood in abdomen & pelvis with active splenic haemorrhage & splenic rupture possibly due to septic spleen and infarction (Fig 1).
An emergency laparotomy & splenectomy was performed. Rifampicin was added to the antibiotic regimen which was continued for 12 weeks on the advice of the Microbiologist. The patient subsequently underwent mitral valve replacement. She made an excellent recovery post surgery & was discharged on penicillin prophylaxis.
Figure 1: Haemoperitoneum and active splenic haemorrhage
Figure 2: Splenic Rupture with active bleeding
Case 2
A 65 year old lady with past medical history of thyroidectomy, hypocalcaemia & ischaemic heart disease presented to her General Practitioner initially with generalised weakness, left upper quadrant and left sided chest pain. She had been discharged only a day before from the medical ward following a treatment for right lung consolidation. The GP found her to be bradycardic and hypotensive and hence referred her to the Cardiac Unit for further assessment.
On admission her heart rate was 50/ minute and blood pressure was 70/45 mm Hg and was in distress because of the left lower chest pain. ECG showed sinus bradycardia with no acute changes. The patient was commenced on IV Fluids & IV antibiotics as her WCC was elevated at 14. Haemoglobin had dropped to 8.6 from 12.6 and hence an urgent CT Abdomen was performed which showed splenic rupture with active splenic bleeding and Haemoperitoneum (Fig 2).
She was resuscitated, transfused with three units of red cells and underwent emergency laparotomy. On opening the abdomen there was large amount of fresh and clotted blood in the upper abdomen and enclosing the spleen. There was brisk significant blood loss from the splenic artery at the hilum. The bleeding vessel was clamped, hilum divided, gastrosplenic ligament clamped and divided and spleen removed. Haemostasis was achieved. The total blood volume removed at the end of the surgery was estimated at 3700 mls. Patient received three more units of red cells and two units of fresh frozen plasma.
Patient was transferred to ICU post surgery, was intubated and ventilated for 12 hours & commenced on IV Cefotaxime, Clarithromycin and Gentamicin for 10 days. The patient remained stable and made a steady recovery.
Serial Blood Cultures for possible infectious cause were negative. Echocardiogram did not reveal any vegetation and the histology from the splenic sample did not show any evidence of infiltration, abscesses or malignancy.
She was commenced on long term Penicillin & vaccines against common encapsulated bacteria and was discharged on eleventh post-operative day. The patient was well on post discharge review.
Discussion
The spleen can be infected in 25-60% of bacterial endocarditis (2). Splenomegaly is clinically found in 33% of the cases. Splenic infarction is seen in nearly 40% of Infective Endocarditis. Staphylococcus aureus and viridans each account for 40% of cases with splenic infarcts and abscesses (2). In our first case the blood cultures grew Staphylococcus sanguis which belongs to viridans group. Abdominal CT/MRI is the investigation of choice with sensitivity and specificity of 90-95%.
Splenic rupture with haemorrhage is a rare complication of splenic infarction. In the series of the Hospital de la Pitie on 120 patients hospitalised with bacterial endocarditis, 5% of them needed splenectomy (3). The basic pathological mechanisms may be rupture of a mycotic aneurysm into the splenic substance, rupture of a splenic abscess and rupture of a suppurating intrasplenic vessel with haematoma formation, subcapsular dissection and delayed capsular tear.
Definitive treatment is splenectomy and this should be performed immediately and before valve replacement surgery because of the risk of infection of valve prosthesis as a result of bacteraemia from the abscess.
In our second case splenic rupture was caused by a splenic artery aneurysm. Splenic artery aneurysms were first described in 1770 by Beaussier.(4) Following the infrarenal aorta and the iliac arteries, the splenic artery is the most common site of aneurysm formation in the abdomen.(5)
They are two to three times more common in females than in males, and they are most often detected in the third and sixth decades of life. Several series have shown a strong association between splenic artery aneurysms and multiple pregnancies. Interestingly our patient was multi gravid (G6, P6).Approximately one-half of all women diagnosed with splenic artery aneurysms were pregnant at the time of diagnosis.(5,6,7) The most common etiologic factor contributing to their formation is medial degeneration with concomitant atherosclerosis.
The overall risk of rupture has been difficult to quantify, since the prevalence of splenic artery aneurysms is uncertain, but the risk is believed to be between 5.3 and 46.0 percent. Rupture is the most common and most serious complication, and 46 percent of patients initially present with massive intraperitoneal rupture.
The mainstay of treatment has been resection of the splenic artery with splenectomy. However, spleen-salvaging procedures are now sometimes performed, depending on the location of the lesion and the presentation of the patient.
References
- Atkinson E. Death from idiopathic rupture of the spleen. BMJ 1874; 2: 403-4
- Gadacz P, Way LW, Dunphy JE: Changing clinical spectrum of splenic abscess. AM J Surg 1974:128:182-187.
- Godeau P, Wescher B, Herreman G, Balafrej M: Rupture de la rate au cours des endocarditis bacteriennes. Nouv Presse Med 1979;8:2811-2814.
- Beaussier M. Sur un aneurisme de l'artere splenique dont les parois se sont ossifiees. J Med Toulous 1770;32:157.
- Abrams HL, ed. Angiography: vascular and interventional radiology. Boston: Little, Brown, 1971: 2(3):1548-58.
- Stanley JC, Fry WJ. Pathogenesis and clinical significance of splenic artery aneurysms. Surgery 1974;76:898-909.
- Stanley JC, Thompson NW, Fry WJ. Spanchnic artery aneurysms. Arch Surg 1970;101:689-97.
Copyright Priory Lodge Education Limited 2007
First Published August 2007
Click
on these links to visit our Journals:
Psychiatry
On-Line
Dentistry On-Line | Vet
On-Line | Chest Medicine
On-Line
GP
On-Line | Pharmacy
On-Line | Anaesthesia
On-Line | Medicine
On-Line
Family Medical
Practice On-Line
Home • Journals • Search • Rules for Authors • Submit a Paper • Sponsor us
All pages in this site copyright ©Priory Lodge Education Ltd 1994-