Common High Altitude Medical Problems
Dr. SS Tan MBBS, FRCA, FAMS |
Dr. VWT CheeMBChB |
<< Previous Page
ABSTRACT
Introduction:
Altitude related medical problems cause significant avoidable morbidity and mortality. Many high altitude places are remotely located and away from medical help. It is imperative for persons travelling to such places to be able to recognize symptoms of common problems and manage them accordingly. This review aims to highlight common altitude related illnesses, their aetiologies and current management.
Methods:
This review is based on research articles, previous reviews and a consensus conference. The search was performed with MEDLINE, from 1968 to 2000. Only currently accepted management based on more recent papers are highlighted. Only papers and books in English were reviewed.
Results:
Tissue hypoxia caused by a reduced ambient partial pressure of oxygen is the
basis for pathophysiological changes in altitude related illness. Acute Mountain
Sickness (AMS) is common and preventable with sensible altitude gain. If it
occurs, AMS is usually mild and self-limiting if it is recognized and managed
properly. Severe and potentially fatal manifestations such as High Altitude
Pulmonary Edema and High Altitude Cerebral Edema must be diagnosed and managed
without delay.
Eye problems are often unrecognized and can cause problems. Myopes with Radial
Keratotomy can experience significant refractive changes and high altitude retinopathy
can be asymptomatic unless the hemorrhages are large and encroach on the macula.
Conclusion:
Altitude related illnesses are common and should be recognized promptly to avoid
unnecessary morbidity and mortality.
KEY WORDS: acute mountain sickness, pulmonary edema, cerebral edema
COMMON HIGH ALTITUDE MEDICAL PROBLEMS
A 45 year old male with a history
of bronchial asthma was travelling with an organized trekking group. They had
flown in to an airstrip at 2800m and spent a few days in the local town before
trekking to 5000m within 3 days. During this time he had complained of mild
headache. The evening after arrival at 5000m, he complained of difficulty breathing
but this was attributed to asthma and was told to rest. The next day, feeling
better, he attempted to walk with the group up to a viewpoint about 100m higher.
He then collapsed and was then put in a portable hyperbaric chamber for 20 minutes.
After a brief period in the bag he struggled and complained of increasing dyspnoea.
The group leader then decided to carry the victim in the bag down the mountain.
After struggling for 6 hours, the group was exhausted and sent a runner to the
nearest village to radio for a helicopter. The patient died soon after. A postmortem
examination done a few days later confirmed the diagnosis of high altitude pulmonary
edema. This case illustrates the importance of early diagnosis and aggressive
management of this condition.
This is a true account; the author's climbing group met the other group's leader
when we arrived at the campsite at 5000m.
This short review will cover only altitude related medical problems and will
not deal with helicopter extraction, cold injuries or travel medicine issues
such as gastrointestinal infections and mosquito borne diseases.
Altitude related illnesses usually occur above altitudes of 3000m (although
the effects may be felt by 2500m). There are many such areas in the world. (Table
1) Some are accessible only to experienced trekkers and mountaineers whilst
others may be visited by the ordinary tourist or traveler.
|
Table I : Areas in the world > 3000m high |
In the Himalayas alone, there is significant morbidity and mortality from altitude related illness. (Table II)1,2
|
British Expeditions to peaks > 7000m 1 Trekking population 2 |
| Table II: morbidity and mortality at high altitude. |
BASIS OF MEDICAL PROBLEMS
The basic problems of high altitude
trips relate to:
a. remoteness of location
b. high altitude effects on the human body
Remote locations make access to medical help difficult if not impossible. The speed of evacuation of injured or ill trekkers or climbers is often dictated by the availability of porters, pack animals or helicopters. The last option being very dependent on the weather, availability of aircraft and last but not least whether the victim possesses a valid insurance certificate.
Altitude related illnesses can be thought of as a spectrum of disorders from the common and relatively mild Acute Mountain Sickness (AMS) to the life threatening forms such as High Altitude Pulmonary Edema (HAPE) and High Altitude Cerebral Edema (HACE). The incidence of AMS varies from 30% 3 to as high as 68%4, with the more severe manifestations of HAPE and HACE varying between 2.5 5 - 5% 4 and 1.8 5 - 31% 4 respectively.
ACUTE MOUNTAIN SICKNESS (AMS)
AMS describes a collection of symptoms
that typically manifests within 6 - 12 h of ascent to altitudes > 2500 -
3000m. Occasionally, symptoms may not appear till a day after ascent. If no
further altitude gain is made, these symptoms usually resolve within 24 - 72h.
The rate at which different individuals acclimatize is extremely variable and
has little bearing on sea level fitness. A recent study found no correlation
between VO2 max and incidence of AMS during a climbing expedition.6
This same study also found no correlation between hypoxic ventilatory response
(HVR) and AMS susceptibility although other studies 7,8 have suggested that
a low ventilatory response to hypoxia and a relatively higher alveolar carbon
dioxide tension (PACO2) increases the risk of AMS.
The barometric pressure decreases in an exponential manner as altitude is gained. (Fig. 1). The pressure at 5800m (e.g. Everest Base Camp) is approximately half that at sea level so that the PO2 of moist inspired gas is 70mmHg, compared with approximately 150mmHg at sea level.9 At the summit of Mt Everest (8848m), the inspired PO2 is only 43mmHg.
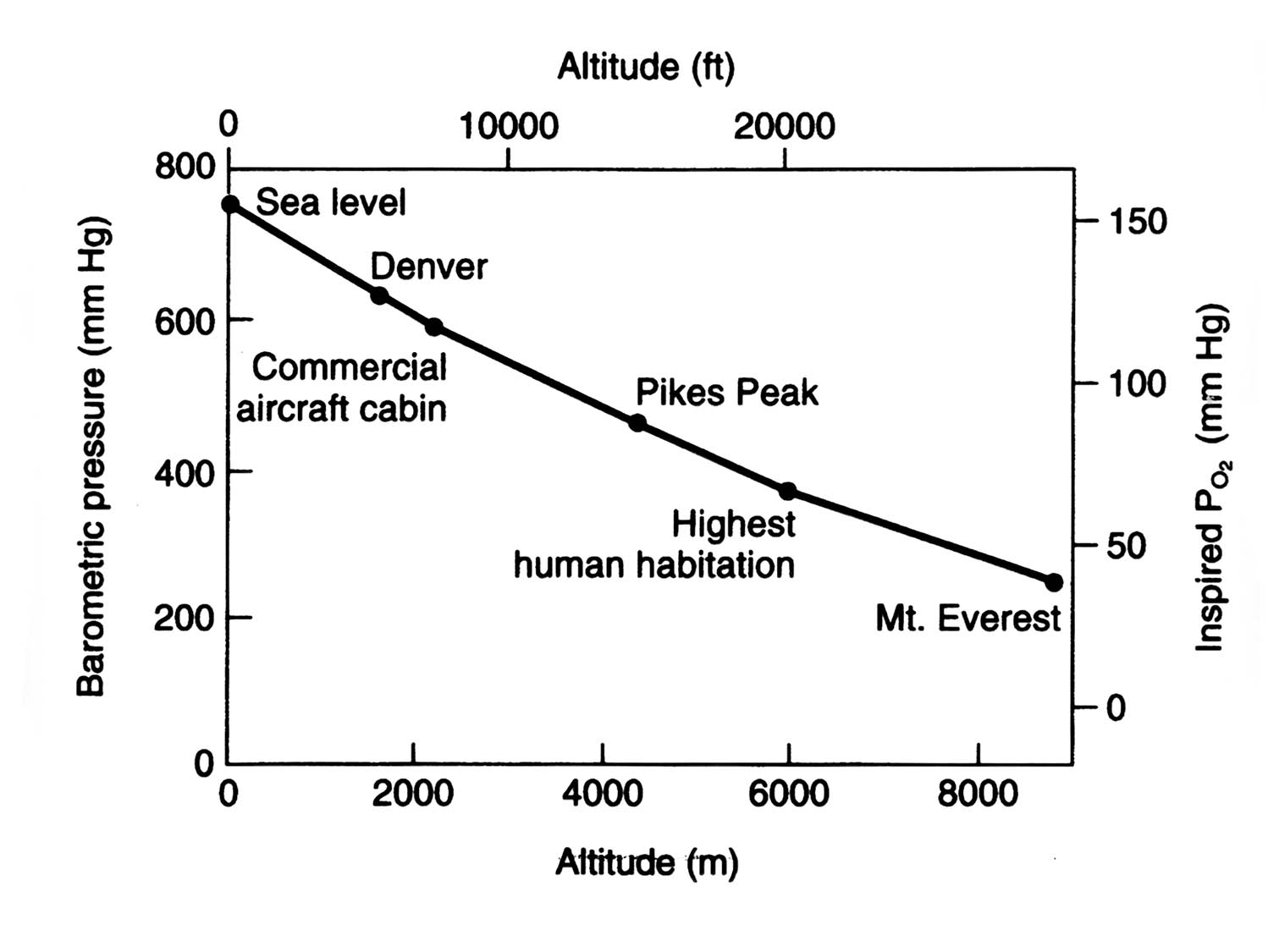
Figure 1. Relationship between altitude and barometric pressure. (Redrawn and reproduced with permission from West JB. Respiratory system under stress. In Respiratory Physiology, The Essentials, 6th ed 1999, pp119-20. Lippincott Williams & Wilkins, Baltimore, MA, USA.) 9
Clearly then, the basis of pathophysiological changes is tissue hypoxia. The greater the hypoxic stress (i.e. the faster the rate of ascent), the less time the body has to adapt to it, the greater the severity of the illness. The possible mechanisms underlying AMS are illustrated in Fig. 2.

Figure 2. Possible mechanisms underlying AMS. ICF, intracellular fluid; ECF, extracellular fluid; CBF, cerebrospinal fluid, ANP, atrial natriuretic peptide. (Reproduced with permission from Ward MP, Milledge JS, West JB. High Altitude Medicine and Physiology, 2nd ed. 1995. p372. Chapman & Hall, London, UK. 10
Diagnosis of AMS
The main symptoms are headache, anorexia,
nausea with or without vomiting, fatigue / lethargy, breathlessness on exertion
and sleep disturbance. These are by themselves non-specific but in the context
of altitude gain, should be interpreted as possible AMS unless proven otherwise.
There is usually a paucity of clinical signs.
The Lake Louise AMS Symptom score 11 attempts to make diagnosis simpler. A score
of 3 or more on the questionnaire is positive for AMS. (see Table III)
Table III : The Lake Louise consensus scoring of AMS 11
AMS self assessment |
Symptom Scoring |
| Headache |
0 None at all 1 Mild headache 2 Moderate headache 3 Severe headache, incapacitating |
| Gastrointestinal symptoms |
0 Good appetite 1 Poor appetite or nausea 2 Moderate nausea or vomiting 3 Severe, incapacitating nausea and vomiting |
| Fatigue and/or Weakness |
0 Not tired or weak 1 Mild fatigue/weakness 2 Moderate fatigue/weakness 3 Severe fatigue/weakness |
| Dizziness/light-headedness |
0 None 1 Mild 2 Moderate 3 Severe, incapacitating |
| Difficulty sleeping |
0 Slept as well as usual 1 Did not sleep as well as usual 2 Woke many times, poor night's sleep 3 Could not sleep at all |
| Overall, if you had any of
these symptoms how did they affect your activities ? |
0 Not at all 1 Mild reduction 2 Moderate reduction 4 Severe reduction (bedrest) |
Prevention of AMS
The usual recommendation is modest
altitude gains of not more than 300m per day above 3000m and to spend 2 nights
in the same place every 1000m 12. This rule of thumb has been widely quoted,
and most trekkers appear to acclimatise reasonably with this rate of ascent,
although a minority do not acclimatise well. Recently, a suggestion has been
made to spend a night or two at intermediate altitudes below 3000m before ascending
further 13.
Drug prophylaxis using acetazolamide is well established 14,16,17,18. However,
this is not a substitute for gradual ascent. It is usually recommended only
for those who have shown to be susceptible to AMS, or who have to make large
altitude gains over a short period, e.g. military or rescue personnel, or tourists
flying into high altitude destinations such as Leh, Ladakh (3514m) or Lhasa
(3658m). The current dose recommendations made by the Himalayan Rescue Association
(Phone: 262746 Thamel Mall Building, Jyatha Thamel, Kathmandu, Nepal) is 125mg
BD. This dose is as effective as the previously recommended dose of 250mg BD
whilst reducing the unpleasant side effects of tingling of hands and feet and
diuresis. Since acetazolamide is a diuretic, the trekker or climber is well
advised to make efforts to drink enough liquids to remain well hydrated, as
dehydration appears to hamper acclimatisation as well. Acetazolamide, a carbonic
anhydrase inhibitor is a sulpha drug and should be avoided by those with sensitivity
to sulpha drugs. It produces a mild metabolic acidosis 18,19 and stimulates
respiration, leading to an increase in alveolar PO2 14 and improves sleep quality
at altitude18,19.
Treatment of AMS
The treatment of AMS is summarised in Table 3. Principles of management are; if in doubt, treat as for AMS; stop further ascent, treat headache with simple analgesics such as paracetamol, rest and rehydrate. Descend if there is no improvement or if symptoms worsen. Immediate descent / evacuation if there are symptoms and signs of HAPE or HACE, with concomitant initiation of pharmacological therapy. Note that the use of hyperbaric chamber should not delay descent / evacuation unless movement in adverse weather conditions imposes an even greater risk of morbidity to both patient and rescuers.
| TREATMENT OF AMS |
| Mild : Rest ( no further altitude
gains ) Symptomatic treatment e.g. paracetamol for headache Severe : DESCENT Oxygen Acetazolamide 250mg 8h, PO14 Dexamethasone 4mg 6h, PO or IM/IV 15 Hyperbaric chamber |
TABLE IV : Treatment of AMS
HIGH ALTITUDE PULMONARY EDEMA (HAPE)
HAPE can occur within 24 - 48h after ascent to 3000m in susceptible people, the risk of increasing with greater sudden altitude gains. It is usually preceded by symptoms of AMS. It is associated with raised pulmonary artery (PA) pressures, 20, 21 and high protein lung lavage fluid 22, 23. It is made worse by physical exertion, and relieved by nifedipine 20, oxygen and rest. Typically, the person experiences diminishing effort tolerance, to the point of being breathless at rest. A cough, initially dry will become wet and productive. Auscultation of the lungs reveals crackles. With poor gas exchange, the patient becomes increasingly cyanosed. HAPE is a medical emergency. The mainstay of treatment ( Table 3 ) is immediate descent of at least a 1000m or to below where the person was last asymptomatic. Deaths have occurred when diagnosis or descent was delayed. Nifedipine 10mg stat (sublingual) followed by 10 - 20mg SR 6h should be started. Oxygen if available improves symptoms. As exertion and cold increase PA pressure, the person should be assisted or carried and kept warm. Hyperbaric bags or portable altitude chambers (PAC) may be used if there is no means of safely evacuating the person but should never delay descent. If the HAPE victim is treated in a PAC, he should be maintained in a position of slight (30°) head up tilt to reduce orthopnoea. If HACE is also present, dexamethasone should also be given. The use of acetazolamide in this instance may worsen the tachypnoea.
| TREATMENT OF HAPE |
| 1. DESCENT ! 2. Nifedipine 10mg SL stat, 10-20mg SR 6h 3. Oxygen 4. Hyperbaric bag |
TABLE V : Treatment of HAPE
HIGH ALTITUDE CEREBRAL EDEMA (HACE)
HACE is a severe cerebral manifestation of altitude illness 24. Like HAPE, it can be rapidly fatal. Whilst persons with AMS have very mild neurological symptoms, very few actually develop full blown HACE. However, HACE is often associated with HAPE 25. It appears that vasogenic edema in response to hypoxia is a culprit but certain biochemical mediators may play a role in altering the blood brain barrier (BBB) 26. The "tight fit" hypothesis 26 proposes that individual anatomical differences in the craniospinal axis determines tolerance to mild brain swelling and the apparent random nature of HACE 27.
Diagnosis of HACE
HACE should be suspected when a person complains of severe headache, becomes confused, ataxic or irrational. They may become lethargic and sleepy and if left alone in their tents "to sleep it off", may be found comatose or dead the next day. As for HAPE, if in doubt, treat as for HACE and descend immediately. Dexamethasone 8mg stat (PO/IM) and 4mg 6h should be started, oxygen administered if available. A PAC may be used if immediate descent is impossible.
| TREATMENT OF HACE |
| 1. DESCENT ! 2. Dexamethasone 8mg stat, 4mg 6h 3. Oxygen 4. Hyperbaric bag |
Table VI : Treatment of HACE
PORTABLE HYPERBARIC CHAMBERS
Portable hyperbaric chambers which can simulate a descent of approximately several hundred to 1000m have been shown to be useful in the management of altitude illnesses 28,29,30,31. They can best be described as single person chambers constructed from lightweight materials and closed with a zipper producing an airtight seal. There are usually transparent panels though which the patient can be monitored. After the patient is placed inside, the bag is inflated with a foot pump to a preset working pressure. Continuos pumping is necessary to maintain fresh airflow into the bag and prevent carbon dioxide buildup. Three bags are commercially available. The Gamow bag (Portable Hyperbarics Inc., PO Box 510 Ilion, NY 13357, USA) is cylindrical and operates with an internal pressure of 104 mmHg. This will simulate a descent of 500 - 1500m or more depending on the actual altitude at which the person is. Charts are available from the manufacturer but an altimeter placed within the bag is helpful. The CERTEC bag (CERTEC, Sourcieux-les-Mines, 69210, France) is conical and works with an internal pressure of 165 mmHg. For the same actual altitude, it simulates a lower virtual altitude. However, it is a lighter bag to carry (4.8kg vs. 6.5kg). The newest bag on the market is the PAC (CE Bartlett Pty Ltd., PO Box 49, Wendouree, Vic., Australia). The shape is similar to the Gamow bag. Simulated descents of about 2000m are achievable at an operating pressure of 2 psi above ambient pressure.
The minimum treatment time in any of these bags is an hour, after which the patient may be reassessed. Further time in the bag may be required if the patient is still symptomatic. After emergence from the bag, symptoms may recur and it is wise to descend to lower altitude. It cannot be overemphasized that the hyperbaric bag is not substitute for descent. Unfortunately, the provision of such a device by trekking agencies have lulled some groups into a false sense of security and the use of it by persons unfamiliar with the bag has led in certain instances to avoidable morbidity and mortality.
EYE PROBLEMS AT ALTITUDE
Eye problems at altitude are often overlooked. Briefly, they consist of snow blindness, (this is not confined to high altitude), problems of myopes having had radial keratotmy (RK) 32,33,34, and high altitude retinopathy 35.
The amount of UVA and UVB radiation to the eye is greater at altitude than at seal level. This effect is often compounded by rays bouncing of bright snow resulting in snow blindness. The best way to prevent this is the use of proper high altitude sunglasses that filter out all UVA/UVB, up to 70-100% Infra Red (IR) and are much darker than ordinary sun glasses used at sea level. Treatment includes padding the eyes, steroid and lubricant eye drops, a cycloplegic and simple analgesics for pain. Symptoms usually subside in a day or two. Local anaesthetic eye drops are not usually recommended.
It is now well documented that patients who have had RK for correction of myopia experience refractive changes at altitude 32,33,34. These changes range from minor irritations to severe disability 34. In one study 32, after 24 - 48h at altitudes greater than 3000m, study subjects experienced significant, progressive and reversible hyperopic shift. In another study 34 one subject could not read his watch or assemble a cookstove. Reading glasses did not improve near vision. Distance vision was also reduced to 20/50 without correction, which led to difficulty in distinguishing people and terrain features. This same deterioration of vision might have also hampered mountaineer Beck Weathers during the storm on Everest in Spring 1996 in which 8 climbers died. The suggested etiology of these changes is corneal hypoxia, rather than just a change in atmospheric pressure per se. The clinical effect of the hyperopic shift depends on the refractive error after RK and the subjects ability to accommodate 32, 33. Patients with photorefractive keratectomy (PRK) show no such changes on exposure to altitude 32. To date there have been no studies done on the behavior of eyes that have undergone Laser in situ keratomileusis (LASIK).
Retinopathy in the form of retinal haemorrhage often goes unnoticed 35, unless they are large enough to impair vision or occur near the macula. Asymptomatic haemorrhages have been found in patients with HACE and AMS. Suggested etiology include raised intracranial pressure, cerebral blood flow 35 and decreased intraocular pressure. This coupled with extreme physical exertion and valsalva maneuvers during mountain climbing may lead to haemorrhages.
SUMMARY
In summary, altitude related illness is experienced by a significant number of visitors to altitudes greater than 3000m. With a sensible rate of altitude gain, the majority of trekkers will be able to enjoy their high altitude sojourn without untoward effects. However, a minority will go on to develop HACE and / or HAPE. Prompt diagnosis and recognition of these latter problems is imperative to prevent unneccessary morbidity and mortality.
REFERENCES
1. Pollard A; Clarke C. Deaths during mountaineering at extreme altitude [letter] Lancet 1988; Jun 4;1:1277.
2. Shlim DR, Gallie J. The causes of death among trekkers in Nepal. Int J Sports Med 1992; Oct.13 Suppl 1:S74-6.
3. Basnyat B, Lemaster J, Litch JA. Everest or bust: a cross sectional, epidemiological study of acute mountain sickness at 4243 meters in the Himalayas. Aviat Space Environ Med 1999; Sep;70(9):867-73.
4. Basnyat B, Subedi D, Sleggs J, Lemaster J, Bhasyal G, Aryal B, Subedi N; Disoriented and ataxic pilgrims: an epidemiological study of acute mountain sickness and high altitude cerebral edema at a sacred lake at 4300m in the Nepal Himalayas. Wilderness and Environmental Med 2000; 11, 89-93.
5. Hackett PH, Rennie ID, Levine HD. The incidence, importance, and prophylaxis of acute mountain sickness. Lancet 1976; 2: 1149-54.
6. Milledge JS, Beeley JM, Broome J, Luff N, Pelling M, Smith D. Acute mountain sickness susceptibility, fitness and hypoxic ventilatory response. Eur Respir J 1991; Sep;4(8):1000-3.
7. Hackett PH, Rennie D, Hofmeister SE, Grover RF, Grover EB, Reeves JT. Fluid retention and relative hypoventilation in acute mountain sickness. Respiration 1982; 43(5), 321-29
8. Matsuzawa Y, Fujimoto K, Kobayashi T, Manushi NR, Harada K, Kohno H, Fukushima M, Kusuma S. Blunted hypoxic ventilatory drive in subjects susceptible to high altitude pulmonary edema. J Appl. Physiol. 1989; 66(3) : 1152-7.
9. West JB. Respiratory system under stress. In Respiratory Physiology, The Essentials, 6th ed 1999, 119-20. Lippincott Williams & Wilkins, Baltimore, MA, USA.
10. Ward MP, Milledge JS, West JB. High Altitude Medicine and Physiology, 2nd ed. 1995. p372. Chapman & Hall, London, UK.
11. Hackett PH, Oelz O. The Lake Louise Consensus on the definition and quantification of altitude illness. Hypoxia and Mountain Medicine 1992 (Sutton JR, Coates G, Houston CS. eds.).Queens City Printers, Burlington, pp327-30.
12. Ward MP, Milledge JS, West JB. High Altitude Medicine and Physiology, 2nd ed. 1995. p377. Chapman & Hall, London, UK.
13. Murdoch DR. How fast is too fast ? Attempts to define a recommended ascent rate to prevent acute mountain sickness. ISMM Newsletter 1999; 9(1): 3-6.
14. Grissom CK, Roach RC, Sarnquist FH, Hackett PH. Acetazolamide in the treatment of Acute Mountain Sickness: Clinical Efficacy and Effect on Gas exchange. Ann. Intern. Med. 1992; 116: 461-65
15. Ferrazzini G, Maggiorini M, Kriemler S, Bartsch P, Oelz O. Successful treatment of acute mountain sickness with dexamethasone. Br Med. J. 1987; 294:1380-2.
16. Forwand SA, Landowne M, Follansbee JN, Hansen JE. Effect of acetazolamide on acute mountain sickness. N Engl. J Med. 1968 Oct 17;279(16):839-45
17. Forwand SA, Landowne M, Follansbee JN, Hansen JE. Acetazolamide for acute mountain sickness. N Engl J Med 1969; 280(1):49.
18. Swenson ER, Leatham KL, Roach RC, Schoene RB, Mills WJ Jr, Hackett PH, Renal carbonic anhydrase inhibition reduces high altitude sleep periodic breathing. Respir Physiol 1991;86(3):333-43.
19. Sutton JR, Houston CS, Mansell AL, McFadden MD, Hackett PM, Rigg JR, Powles AC. Effect of acetazolamide on hypoxemia during sleep at high altitude. N Engl. J Med.1979; 301(24):1329-31.
20. Oelz O, Maggiorini M, Ritter M, Waber U, Jenni R, Vock P, Bartsch P. Nifedipine for high altitude pulmonary oedema. Lancet 1989; 2:1241-4.
21. Grissom CK, Elstad MR. The pathophysiology of high altitude pulmonary edema. Wilderness Environ. Med. 1999; 10: 88-92.
22. Schoene RB, Hackett PH, Henderson WR, Sage EH, Chow M, Roach RC, Mills WJ Jr, Martin TR. High-altitude pulmonary edema. Characteristics of lung lavage fluid. JAMA 1986; 256(1): 63-9.
23. West JB, Mathieu-Costello O. High altitude pulmonary edema is caused by stress failure of pulmonary capillaries. Int J Sports Med 1992; Suppl 1:S54-8.
24. Houston CS, Dickinson J. Cerebral form of high-altitude illness. Lancet 1975; 2 : 758-61.
25. Hackett PH, Roach RC. High-altitude medicine. Wilderness Medicine, (Auerbach PA, ed.). St Louis, MO: Mosby; 1995: 1-37.
26. Hackett PH. The cerebral etiology of high-altitude cerebral edema and acute mountain sickness. Wilderness Environ. Med. 1999; 10: 97-109.
27. Ross RT. The random nature of cerebral mountain sickness. Lancet 1985; 1: 990-91.
28. Bartsch P, Merki B, Hofsetter D, Maggiorini M, Kayser B, Oelz O. Treatment of acute mountain sickness by simulated descent: a randomised controlled trail. BMJ 1993; 306: 1098-101.
29. Zafren K. Gamow bag for high altitude cerebral edema.[letter]. Lancet 1998; 352:325.
30. Austin D. Gamow bag for acute mountain sickness. [letter]. Lancet 1998; 351: 1815.
31. Keller HR, Maggiorini M, Bartsch P, Oelz O. Simulated descent v dexamethasone in treatment of acute mountain sickness: a randomised trial. BMJ 1995; 310: 1232-35.
32. Mader TH, Blanton CL, Gilbert BN, Kubis KC, Schallhorn SC, White LJ, Parmley VC, Ng JD. Refractive changes during 72-hour exposure to high altitude after refractive surgery. Ophthalmology 1996;103(8):1188-95.
33. Winkle RK, Mader TH, Parmley VC, White LJ, Polse KA,. The etiology of refractive changes at high altitude after radial keratotomy. Hypoxia versus hypobaria.Ophthalmology 1998;105(2):282-6.
34. Mader TH, White LJ. Refractive changes at extreme altitude after radial keratotomy. Am J Ophthalmol 1995;119(6):733-7.
35. Wiedman M; Tabin GC, High-altitude retinopathy and altitude illness. Ophthalmology 1999;106(10):1924-6; discussion 1927
CORRESPONDENCE TO:
Dr. SS Tan
MBBS, FRCA, FAMS
Sen. Consultant
Department of Paediatric Anaesthesia
KK Women's and Children's Hospital
100 Bt Timah Road
S 229899
REP OF SINGAPORE
Tel: 3941091
Fax: 2912661
First Published on February 10th 2001
Version 1.0
Home • Journals • Search • Rules for Authors • Submit a Paper • Sponsor us
All pages copyright ©Priory Lodge Education Ltd 1994-

