Browse through our Journals...
Evaluation of oxygen requirement in patients during Fiberoptic Bronchoscopy
E.Alijanpour(MD)1*, N. Nickbakhsh2
Said Soleymani ( MD) 3, Zahra Yekta (MD)4, Elham-Ahmadnezhad (MD, MPH)5
1.*Assistant Professor of Anesthesiology, Babol University Medical Sciences
2. Assistant Professor of Surgery, Babol University Medical Science
3. Assistant Professor of Anesthesiology, Army Tehran Medical University
4. Associate Professor of Community Medicine Urmia University of Medical Sciences
5. Researcher, Urmia University of Medical Sciences
Abstract
In some centres oxygen is given to all patients during fiberoptic bronchoscopy to prevent arterial hypoxemia but in other centres oxygen is given to patients with an SPO2 less than 90%.
Regarding to different opinions in this matter, we evaluate patients oxygen requirement according to SPO2 & its relationship with PFT.
Method
In this clinical Trial study, 146 patients who needed fibrberoptic bronchoscopy, were evaluated without age, sex & type of disease limitation from January to april 2007 in Beheshti hospital Babol, IRAN.
Spirometery was performed before bronchoscopy & patients were divided to three groups: FEV1> 2lit, FEV1 between 1-2 lit & FEV1<1lit
Oxygen was given to every patient with SPO2 less than 90% which lasted more than 20 sec during bronchoscopy.
Findings
Eight patients (5.5%) out of 146 needed to oxygen which 33.3% of them had FEV1<1lit (P<0.06) and 26.7% had obstructive PFT pattern (P<0.004).Average age of patients who need oxygen were 66.7± 12.5 years old & patients without O2 requirement were 51.9± 17.7 years old.
Conclusion
According to this study findings, it is recommended to give oxygen during fiberoptic bronchoscopy for old patients, patients with FEV1<1lit & obstructive PFT.
Key words: Fiberoptic bronchoscopy - Oxygen - Hypoxemia
Introduction
In order to treat pulmonary diseases, physicians traditionally used clinical, radiological and laboratory findings.
As technology has progressed, other methods such as pulmonary function tests (PFT) came to help the diagnosis of the disease, evaluation of lung volumes and therapeutic effects .1-2
Bronchoscopy, an invasive method of diagnosis and treatment, was first used by Mr Gustav Killan. Although both kinds of bronchoscopy - rigid and fiberoptic - are used for a more precise diagnosis, easier biopsy and treatment in lung disorders for some time now. 3-5
Even though fiberoptic bronchoscopy is invasive, it can be applied in conscious patients with or without sedation.6-7-8
Most side effects of this bronchoscopy are transient with an incidence rate of 2-3% .12-13
Cough & bronchospasm are the most common side effects of fiberoptic bronchoscopy, which can be reduced by administration of β agonist drugs.10 Another side effect of fiberoptic bronchoscopy, arterial hypoxemia during procedure, can be prevented by O2 administration to all patients, as practiced in some centres, where as oxygen saturation control (SPO2<90%) and decide individually as in other centres. .4-5-7-8-9-10-13 Regarding different opinions in this matter, this study was designed to evaluate the patient’s need for O2 according to SPO2 and its relation to PFT, age and sex.
Methods
In this clinical trial study, 146 patients in need of fiberoptic bronchoscopy who were admitted to Beheshti hospital, Babol medical university from January to april 2007, were enrolled regardless of age, sex & disease type. Patients who contraindicate for fiberoptic bronchoscopy such as uncontrolled asthema, hypoxemia, recent M.I & hypercarbia have been excluded.
After obtaining written informed consent from the patients , PFT was performed for all of them which divided the patients into 3 groups of FEV1 higher than 2 lit , 1-2 lit and less than 1 lit.
The patients were put in the bronchoscopy position and monitored with NIBP and pulse oximeter (CLV-U 40) before, during and 5 minutes after fiberoptic bronchoscopy.
All fiberoptic bronchoscopies were performed with local anesthesia (lidocaine) by one specialist.
Oxygen was given to every patient with SPO2 less than 90% for more than 20 sec through nasal catheter. finally the relationship between patients who had got oxygen and age , sex , spirometery was evaluated statistically by using SPSS software and T-Test fisher's exact & differences between any point of data's with P<0.05 were considered significant.
Findings
Among 146 patients studied 92(63%) were male and 54(37%) female , ranging from 17 to 89 years old with an average of 52.79± 17.79 years old. FEV1 in 88 patients (60.3% )was more than 2 lit , in 49 patients (33.6%)between 1-2 lit and in 9patient(6.2%) less than 1lit. with regards to PFT , 18 patients (12.3%) had restrictive pattern , 15 patients (10.3%) obstructive , 17 patients (11.6%) had mixed pattern and in 96 patients (65.8%) PFT was normal.
The mean SPO2 before bronchoscopy was 96.7 ± 2.6% during bronchoscopy 93.6 ± 3.1% and immediately after bronchoscopy was 94.6 ± 3.6%, which had no significant difference.
In this study, nasal oxygen was administered only to 8 patients (5.5%). (fig1). According to table 1, the need to oxygen in patients with a FEV1 less than 1 lit was significant when compared to patients with FEV1 between 1-2 lit (P<0.042) and more than 2 lit (P<0.005) . On the other hand, there was no significant difference in need of oxygen between patients with FEV1 between 1-2 lit and those with FEV1 more than 2 liters (P=0.349).
There was no relationship between oxygen requirement & sex (Fig-2). As shown in table 2 & 3, the need of oxygen in patients with obstructive pattern in PFT was significantly higher when compared to other patterns (P<004) .Besides, the mean age of patients in need of O2 was significantly higher than those with no need of oxygen , 67 years old in comparison to 52.
Table1: number and % of oxygen requirement in regard to FEV1
Total |
No |
Yes |
oxygen requirement
FEV1/ lit |
|
|||
% |
n. |
% |
n. |
% |
n. |
|
|
100 |
88 |
97.7 |
86 |
2.3 |
2 |
2 > |
|
100
|
49 |
93.9 |
46 |
6.1 |
3 |
1-2 |
|
100
|
9 |
66.7 |
6 |
33.3 |
3 |
<1 |
|
100
|
146 |
94.5 |
138 |
5.5 |
8 |
Total |
|
Table2: number and % of oxygen requirement in regard to PFT pattern
P Value |
Total |
No |
Yes |
Oxygen need
Pattern |
|||
|
% |
no. |
% |
no. |
% |
no. |
|
0.597 |
100 |
18 |
100 |
18 |
- |
- |
Restrictive |
0.004 |
100 |
15 |
73.3 |
11 |
26.7 |
4 |
Obstructive |
0.053 |
100 |
17 |
82.4 |
14 |
17.6 |
3 |
Mixed |
0.002 |
100 |
96 |
99 |
95 |
1 |
1 |
Normal |
|
100 |
146 |
94.5 |
138 |
5.5 |
8 |
Total |
Table3: Mean age of patients in regard to oxygen requirement
P Value (T-Test) |
Mean |
SD ± |
n. |
oxygen requirement
|
0.022 |
51.9 |
17.7 |
138 |
No
|
66.7 |
12.5 |
8 |
Yes
|
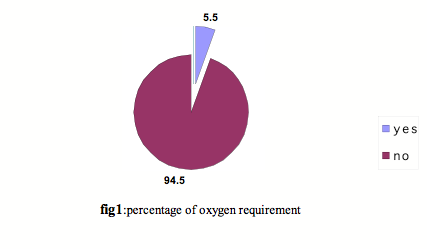
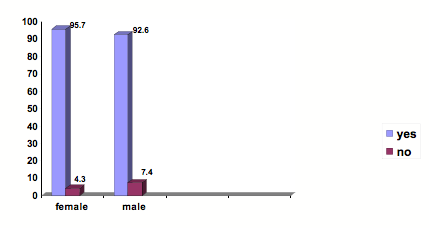
Fig.2: percentage of oxygen requirement in regard to gender
Discussion
Bronchoscopy is an Invasive method for diagnosis & treatment.3 Today fiberoptic bronchoscopy plays an important role in diagnosis & treatment of the patient and in some cases it is the only way of evaluation.5-12
Hypoxemia is a side effect of this method and in order to prevent it, in some centres oxygen is administered to all patients whereas in other centres oxygen is given to patients with SPO2 less than 90%.10 our study which was performed under SPO2 monitoring, showed that only 8 patients (5.5%) out of 146, had a SPO2 less than 90% for more than 20 sec and needed oxygen.
Among the patients in need of oxygen, 33.3 percent were patients with FEV1 less than 1 lit and 26.7 percent were patients with obstructive PFT pattern. Also our study showed that the rate of SPO2 during bronchoscopy is reduced when compared to before and after the procedure but this difference wasn't significant.
In study by Dr. Afsar and his colleagues in 1992, patients were divided into two groups and 50% of them received oxygen during bronchoscopy .The result shows a decline in SPO2 in both groups, but, it was less in the patients receiving oxygen.15
Another study by Rafael shows that obstructive pattern of PFT is one of the most important factors for hypoxemia.16 Study of Evans & his colleagues, in 1998 shows a decrease in Sao2 and an increase Paco2 during bronchoscopy.17
A study in 2000 by Anderew and his associates shows that 24% of patients had SPO2 less than 90% during bronchoscopy but in 14.4 % of patient the decrease of SPO2 lasted for 20-30 sec which received oxygen. According to their report, there is no relationship between FEV1 and fall in Sao2.18 Another research in 1998 by kristensen MS and his co-workers shows that the amount of FEV1 is one of the most important clinical factor for prediction of hypoxemia during fiberoptic bronchoscopy.19 Dr Milman & his colleagues study indicates that increased age has an effect on decrease of SPO2 and pulse oximeter is a good monitoring for diagnosis of hypoxemia.20 According to Dr sharma and his associates study in new Dehli on 21patients, with ABG evaluation, they reported that all patients need oxygen therapy during bronchoscopy. 21
In 2002 a research by pinar shows that, there is no difference between amount of oxygen saturation in ABG and Pulse oximeter & one of the most important factors in decrease of SPO2 is the duration of bronchoscopy. They recommended pulse oximeter monitoring for all patients and in cases of prolonged bronchoscopy oxygen therapy is needed.22
Conclusion
This study and similar other studies show that pulse oximeter is a good monitoring for diagnosis and treatment of hypoxemia during bronchoscopy. Although SPO2 decrease happens in all patients during bronchoscopy, but the need to oxygen is more in patients with FEV1 less than 1 lit, obstructive PFT pattern or elderly, in comparison to the others.
References
1. Gregg L. Ruppel. Mannual of pulmonary function testing. Eight edition. Philadelphia, Lippincott: 2003: PP: 1-10
2.C.Guyton.A. Mall.J Text Book of Medical physiology;ninth edition;Philadelphia;1996;PP:480-497
3. Kitmural S. History of bronchoscope, in: Kitamura S. color at lasot clinical application of fiberoptic bronchoscopy, stlouis- mosby. 1990; PP. 7-8.
4- Jeanne M. Lukanich, David J. sabiston. The text book of surgery. I 7th edition. Sunders 2004: P.P 1784-1786.
5. Steven M. Feinsilver, Alan M. Fein. The text Book of bronchoscopy. 2nd Edition Philadelphia 1996; PP:1-40
6. Ernst A; Silvestri GA; Johnstone D. Interventional pulmonary procedures:Guidelines from the American College of Chest Physicians. Chest 2003 May; 123(5):1693-717.
7. Sway MS, Jayakyishnan B, Behbehani N, Abel AT, EL-Shame A, Nail MG. Flexible fiber optic bronchoscope- Diagnostic yield Saudi Med J-2004 oct; 25(10): 1459-63
8. Schellhase DE, Few cett DD, Schutse GE, Lensing sy, try ka AF. Clinical utility of flexible bronchoscopy and bronchoalveolar lavage in young children with recurrent wheezing. J pediatr.1998 Feb; 132(2): 312-8
9. Thompson A Rennard S. Diagnostic procedures not involving pleura, in :Baum G: Grapoj GelliB, Karlinsky S. Pulmonary diseases, 6th edition Philadelphia, Lippincott. 1998: PP 240-244
10. Jeffrey M. Drazen, steven E, Weinberger Harrison’s principles of internal medicine. Fifth Edition MC Graw-Hill. 2002. P.P: 1450-1455
11. Arroliga AC.Matthay RA. The role of Bronchoscopy in Lung cancer clin chest Med 1993; 14: 87-98
12. Torres A/Serra Batles J, Fetrera/ etal/ severe community acquired pneu monia- epidemilogy and proqnostic factors. Am Resp Dis 1991; (144): 312-318
13. Sinha S, Guleria R, Panda JN, Pander KM. Bronchoscopy in adults at a tertiary care centre: indications and complications. J Indian med Assoc. 2004 Mar; 102(3): I 52-4
14. Barbato A, Magarotto M, Crivellaro M, Novello JrA, Cracco A, De Blic J, et al.. Use of the pediatric bronchoscope, flexible and rigid in 51 European centres. Eur Respir J 1997; 10: 1761-6.
15. Afsar s, choudhri AN, Farooqi T, Pasha MJ. Oxygen desaturation during fiber optic bronchoscopy. J pak Med Assoc.1992 Nov; 42(11): 263-5
16. Rafael G, Alfonso M. Supplemental oxygen during flexible bronchoscopy Chest 2002;121: 664-665.
17. Evans EN, Ganeshalingamk, Ebdenp. Changes in oxygen saturation and transcutaneous carbon dioxid and oxygen levels in patients undergoing fiberoptic bronchoscopy. Respir med. 1998 may; 22(5): 739-42
18. Anderew M. Jones. MB and Ronan o’ Dris coll. Do all patients require supplemental oxygen during flexible bronchoscopy? Chest.2000; 119: 1906-1909.
19. Kristensen MS, Mitman N, Jarnvig IL Pulse oximetry at fiberoptic bronchoscopy with local anesthesia: indication for postbronchoscopy oxygen supplementation? Respir Med (1998); 92: 432-437
20. Milman N, faurschou P, Grode G, Jorgensen A. Pulse oximetry during fiberoptic bronchoscopy in local anaesthesia: frequency of hypoxaemia effect of oxygen supplemtation Respiration. 1994; 61(6) 342-7
21. sharma SK, Pande JN, sakar R. Effect of routine fiberoptic brocchoscopy and bronchoalveoar lavage on arterial blood gases. Indian J chest Dis Allied Sci. 1993 jan mar; 35(1): 3-8
22. Pinar Y, Akif Ö. Changes in oxygen saturation in patients undergoing fiberoptic bronchoscopy. Chet 2002; 121:1007-1008.
Copyright Priory Lodge Education Limited 2007
First Published October 2007
Click
on these links to visit our Journals:
Psychiatry
On-Line
Dentistry On-Line | Vet
On-Line | Chest Medicine
On-Line
GP
On-Line | Pharmacy
On-Line | Anaesthesia
On-Line | Medicine
On-Line
Family Medical
Practice On-Line
Home • Journals • Search • Rules for Authors • Submit a Paper • Sponsor us
All pages in this site copyright ©Priory Lodge Education Ltd 1994-


