Management of post meal hyperglycaemia in patients with type 2 diabetes in a District General hospital in the United Kingdom.
Authors: (1) Indrajit Talapatra (MRCP): Speciality Doctor in Diabetes/Medicine, Royal Albert Edward Infirmary, Wigan WN12NN, UK
Email: indratala@aol.com
(2) Eleanor O’Brien (MBCHB): Foundation year doctor, Department of Medicine, Royal Albert Edward Infirmary, Wigan WN12NN,UK
(3) Avraneel Talapatra: Medical School, University of Manchester, M13 9PT, UK
(4) David James Tymms (FRCP) Consultant in Diabetes/Medicine, Royal Albert Edward Infirmary, Wigan, WN12NN, UK
Introduction: Post meal hyperglycaemia is known to be an independent risk factor to cause complications despite a good level of glycosylated haemoglobin (HbA1C) which gives no information on the extent or frequency of blood glucose excursions.
Post meal hyperglycaemia begins prior to the onset of type 2 diabetes. It is very important to keep the post meal blood glucose level below 7.8 mmol/l (140 mg/dl). High post meal blood glucose levels can cause increased risk of retinopathy, increased carotid intima-media thickness, increased oxidative stress and endothelial dysfunction, decreased myocardial blood flow, increased risk of pancreatic cancer and decreased cognitive function in elderly population (1).
Prior to onset of clinical diabetes there is loss of first-phase insulin secretion together with decreased insulin sensitivity in peripheral tissues and there is decreased suppression of hepatic glucose output due to insulin deficiency (2,3,4). Loss of post meal glycaemic control precedes step wise deterioration in nocturnal fasting periods with worsening diabetes (1). High post meal sugars are related to deficiencies in amylin (a glucose regulatory peptide secreted by the B cells of pancreas), GLP-1 (Glucagon-like Peptide-1 secreted by L cells of small intestine) and GIP (Gastric-inhibitory Polypeptide, an insulinotropic peptide secreted by K cells of the small intestine)., (5,6)
Aims: To find out whether post meal glucose control was good in patients with Type 2 diabetes and to increase awareness amongst patients of its significance.
Methods: Case notes of the last fifty-two patients with Type 2 diabetes seen for annual review prior to preparation of the audit in April 2013 were studied. The standards used were according to the recommendations of IDF (International Diabetes Federation)..
Standards: The guidelines of IDF 2008, revised in 2011, were taken into consideration (1).
- To implement treatment strategies to lower post meal plasma glucose in people with post meal hyperglycaemia
- Dietary intake: Foods with lower GI or glycaemic index (a measure of how quickly blood sugar rises after consumption of a certain type of food) such as legumes, pasta and fruits should be consumed. Low dietary glycaemic load or GL (the product of the carbohydrate content of the diet and its average GI) should be taken into consideration
- Pharmacological agents to be used for lowering post meal plasma glucose are as follows: Alpha -glucosidase inhibitor (Acarbose), Glinides (insulin secreting agents such as Repaglinide and Nateglinide), Amylin analogue (Pramlintide), DPP-4 (Dipeptidyl Peptidase) inhibitors or Gliptins, GLP-1 analogues, short acting Sulfonylurea Glipizide and short acting and mixed insulins.
- Post meal glucoseafter 2 hours should not exceed 7.8 mmol/l as long as hypoglycaemia is avoided
- SMBG (self-monitoring of blood glucose) should be considered because it is currently the most practical method for monitoring post meal hyperglycaemia. It is generally recommended that in patients treated with insulin, SMBG should be performed at least three times daily whereas SMBG frequency for people not treated with insulin should be individualized to each person’s treatment regimen and level of control
- Efficacy of treatment regimens should be monitored as frequently as needed to guide therapy towards achieving post meal plasma glucose target.
Standards against which the audit was performed:
- Patients had seen a dietician within the last 3 years
- Those who had seen a dietician were aware of food with low GI and GL
- The patients were on proper pharmacological agents
- Post meal glucose level were monitored by proper SMBG in those who were on oral treatment
- At least three times daily SMBG was done by patients on insulin
- Target level of 7.8 mmol/l (140 mg/dl) of 2- hour post meal glucose was achieved
Age distribution: Total number of patients 52 (n=52); 40-50 years= 14 patients; 50-60 years =12 patients; 60-70 years=20 patients; 70-80 years= 6 patients
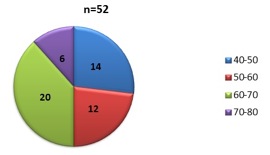
Graph 1: pie chart showing age distribution of the studied population
Sex distribution: Male= 22 patients; Female=30 patients
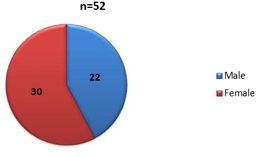
Graph 2: pie chart showing sex distribution of studied population
Results: Table 1
Patients had seen a dietician within the last 3 years |
8 patients (15.4% of total number), see graph 3 |
Reasons: Remaining patients did not receive invitation from the dietician |
Patients who had seen a dietician were aware of food with low GI and GL |
6 out of 8 |
|
The patients were on proper pharmacological agents |
30 (56.7% of total) were on insulin (short acting and mixed insulins); 18 of the remaining 22 patients were on Gliptins or GLP-1 analogues as part of combination therapy (see graph 4) |
Remaining 4 of 22 patients on oral agents only were on Metformin and/or Sulfonylureas (like Gliclazide) but not on Glipizide |
Whether SMBG were done by patients, not on insulin, post meal |
6 out of 22 (27.3% of those on oral hypoglycaemics), see graph 5 |
Of the remaining 16 patients, 8 patients were doing blood glucose monitoring in the morning and another 8 patients in the morning and bedtime. |
Whether patients on insulin were doing SMBG thrice daily including post meal |
25 out of 30 (83.3% out of those on insulin), see graph 6 |
3 of the remaining 5 patients were doing SMBG in the morning and at night and 2 patients only in the morning |
Post meal level of blood glucose of 7.8 mmol/l was achieved |
10 patients had HbA1C less than 7.8mmol/l or 140 mg/dl (see graph 7) |
Remaining patients did not achieve the target and were not aware of the significance of post meal glucose target or its significance. However most of them were aware of the importance of HbA1c and its normal level |
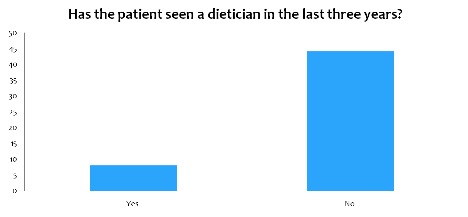
Graph 3: bar chart showing distribution of studied population who saw a dietician in the last three years
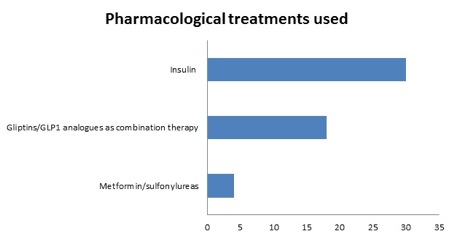
Graph 4: chart showing the different treatments used in the studied population

Graph 5: chart showing proportion of patients on oral hypoglycaemia who were doing self-monitoring of blood glucose
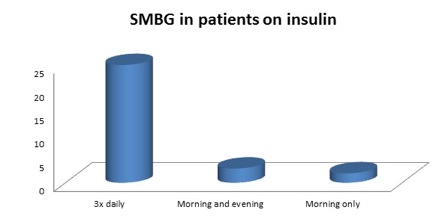
Graph 6: chart showing self-monitoring of blood glucose in patients on insulin
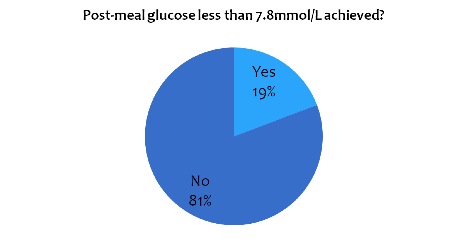
Graph 7: pie chart showing the proportion of patients who achieved the target of post-meal blood glucose
Conclusions:
- Post meal blood glucose control of the patients was poor.
- Most patients were not aware of the significance of high post meal blood glucose level although we found that most of them were aware of the significance of HbA1c levels
- Those on oral hypoglycaemic agents did SMBG only infrequently
- Those on insulin did SMBG quite regularly
- Patients saw dieticians infrequently and hence mostly were not aware of the concepts of GI and GL
- Most patients on oral hypoglycaemics were on post meal blood glucose lowering agents like DPP-4 inhibitors or GLP-1 analogues as part of combination therapy (with Metformin and/or sulfonylureas like Gliclazide or Glimepiride).
Summary and Recommendations: Analysing the outcome of the audit we found that most patients were not aware that post meal hyperglycaemia could be an independent risk factor to cause various complications. In the United Kingdom and worldwide, patients with type 2 diabetes get their HbA1c and fasting blood sugars monitored at variable intervals, usually every 3-6 months. There is not much awareness how important post meal SMBG is. This problem is further compounded by the fact that owing to financial constraints most GP (General Practitioner) surgeries in the UK tend to issue a limited number of strips for capillary glucose monitoring in patients with type 2 diabetes. According to NICE (National Institute of Clinical Excellence) guidelines strips for SMBG should be available to those on oral glucose lowering medications (7) and the Diabetes UK Positional statement clearly mentions that people with Diabetes (both type1 and type2) should have access to SMBG based on their individual clinical need and not the NHS’s ability to pay (8). Patients should also have regular dietician review and learn the importance of targeting post meal blood glucose to less than 7.8 mmol/l. Patients on oral glucose lowering agents need to monitor their day time post meal blood glucose at least 3-4 times a week. .We hope that at the time of re-audit after a year, we will come up with a much better performance.
We know now that HbA1c is not a good biochemical measure for the extent and frequency of high post meal blood glucose excursions. HbA1c is impacted by both fasting and post prandial blood sugars and can show a good result as a result of combination of low-normal fasting blood glucose and high post meal blood glucose levels. Serum 1,5 anhydroglucitol (1,5 AG) drops as plasma glucose rises above its renal threshold (9) and has been proposed and approved by FDA (Food and Drug Administration of USA) as a marker for post prandial hyperglycaemia (10). Perhaps in the future with its regular use together with CGM or continuous glucose monitoring (11), a better monitoring and control of post meal blood glucose will be possible. Optimal blood glucose control cannot be achieved without adequate management of post meal plasma glucose. Therefore treatment of fasting and post meal hyperglycaemia should be initiated simultaneously at any HbA1c level.
References:
- Guideline for management of Post meal glucose: IDF http://www.idf.org/webdata/docs/Guideline_PMG_final.pdf
- Weyer C, Bogardus C, Mott DM, Pratley RE (1993). The natural history of insulin secretory dysfunction and insulin resistance in the pathogenesis of type 2 diabetes mellitus. J Clin Invest. 104(6), 787-794
- Pratlet RE, Weyer C(2001). The role of early impaired insulin secretion in the pathogenesis of type 2 diabetes mellitus. Diabetologia. 44(8), 929-945
- Jerich JE(1996). Pathogenesis and treatment of type 2 (noninsulin-dependent) diabetes mellitus (NIDDM). Horm Metab Res. 28(9), 404-412
- Holst JJ, Gromada J. Role of incretin hormones in the regulation of insulin secretion in diabetic and non diabetic humans(2004). Am J Physiol Endocrinol Metab. 287 (2), E199-E206
- Toft-Nielson MB, Damholt MB, Madsbad S, Hilstead LM, Hughes TE, Michelsen BK et al (2001). Determinants of the impaired secretion of glucagon-related peptide-1 in type 2 diabetic patients. J Clin Endocrinol Metab. 86(8), 3717-3723
- Type 2 Diabetes – Newer agents. Nice Clinical Guideline May 2009
- Self monitoring of blood glucose (SMBG) for adults with type 2 diabetes, April 2013; https://www.diabetes.org.uk/Documents/Position%20statements/Diabetes-UK-position-statement-SMBG-Type2-0413.pdf
- Yamanouchi T, Ogata N, Tagaya T, Kawasaki T, Sekino N, Funato H et al (1996). Clinical usefulness of serum 1,5-anhydroglucitol in monitoring glycaemic control. Lancet. 347, 1514-1518
- McGill JB, Cole TG, Nowatzke W, Houghton S, Ammirati EB, Gautille T et al (2004). Circulating 1,5-anhydroglucitol levels in adult patients with diabetes reflect longitudinal changes of glycaemia: a US trial of the Glycomark assay. Diabetes Care. 27(8), 1859-1865
- Garg S, Zisser H, Schwartz S, Bailey T, Caplan R, Ellis S et al (2006). Improvement in glycaemic excursions with a transcutaneous, real time continuous glucose sensor: a randomised control trial. Diabetes Care. 29(1), 44-50
Declaration: This article is not under consideration for publication in any other Journal. All the four authors contributed towards the preparation of the audit.
Conflict of Interest: None
We did not receive any grant from any Medical Company for preparation of the audit
First Published January 2014
Copyright Priory Lodge Education Limited 2014 -
All pages copyright ©Priory Lodge Education Ltd 1994-


