Browse through our Journals...
Assessment of Neck Lumps
With a significant number of patients visiting their family practitioner for a lump in the neck, we have given an overview of managing these patients in primary care. The important factors to consider are:
1) Normal or abnormal lumps
2) Age
3) History
4) Physical Examination.
Normal or abnormal?
It is important to recognise normal neck masses. The presence of multiple, small, nontender and mobile lymph nodes in children are considered as normal. The hyoid bone, submandibular gland and the transverse process of the first cervical vertebrae can be felt in some people.
Age
In the paediatric age group (0 – 15), a neck lump is likely to be inflammatory followed by congenital lumps and neoplastic lesions. Patients in the age group between 16-40 years are again more likely to have inflammatory lesions followed by congenital and neoplastic lesions. In patients over 40 years of age, a neck lump is to be considered malignant until proven otherwise.
History
The important information to be gathered while history taking is:
1) Onset: The nature of onset is vital to establish the pathology of the lump. A rapid onset painful swelling suggests an inflammatory condition on the other hand a slowly
Progressive lump, which is not painful, suggests a neoplastic lesion. Inflammatory swellings in the neck are commonly associated with infections in the ear, nose, throat and scalp.
2) Duration: Inflammatory lumps settle once the primary source of infection is treated. A neck lump which is persistent (> 6 weeks) with or without associated symptoms needs referral to an ENT surgeon.
3) Associated Symptoms: It is vital to gather information from the patient that would suggest a primary head and neck malignancy causing a metastatic lymph node enlargement. The symptoms and their associations are:
a) Dysphonia (cancer of the larynx)
b) Dysphagia (cancer of the pharynx and oesophagus)
c) Dyspnoea (lung cancer)
d) Weight loss (cachexia)
4) Social History: Occupational exposure to asbestos, nickel and wood dust are associated with an increased risk of head and neck cancers. Smoking is the single most important risk factor for cancers of the upper aerodigestive tract and a detailed history regarding the same should be sought. Alcohol consumption is also a known risk factor for cancers of the head and neck.
Physical Examination
Midline lumps
The most common midline lumps are:
1) Thyroglossal cysts are usually found at the level of the hyoid bone or thyroid cartilage. They move upward on swallowing and on protrusion of the tongue.
2) Thyroid lumps are midline swellings but also present as lateral lumps if one
Lobe of the thyroid is involved. They are more common in adults and in
Females.
2) Dermoid cysts are found at or above the level of the hyoid bone although
they can be found much lower in the neck as well. They do not move upward
on swallowing or protrusion of the tongue.
Lateral Neck Lumps in Children
The majority of neck lumps in children are reactive lymph nodes secondary to infections in the head and neck. They usually settle between 4 and 6 weeks. Solitary neck masses are usually congenital in origin. The most common one being a branchial cyst. A branchial cyst presents as a lump at the junction of the upper one third and lower two third of the sternocleidomastoid. Cystic hygromas present as congenital swellings as well. Neoplastic lumps in children are usually due to a primary cancer (e.g. sarcoma and lymphoma).
Lateral Neck lumps in Adults
As in children the majority of neck lumps in adults are inflammatory as well. Almost all of them settle between 4-6 weeks. Metastatic neck nodes may be the first presenting sign of an underlying malignancy. Any persistent lump (> 6 weeks) should be considered malignant until proven otherwise and needs urgent referral for an ENT assessment. Parotid lumps are classically found below and behind the ear lobule. Thyroglossal and branchial cysts although congenital can also be found in adults.
Neck Triangles
Another common way of describing neck lumps is to divide the neck into two triangles namely the anterior and posterior triangles.
The boundaries of the anterior triangle are
a) Medially: midline of the neck
b) Superiorly: mandible
c) Laterally: Anterior border of the sternocleidomastoid muscle.
The boundaries of the posterior triangle are:
a) Anteriorly: Posterior border of the sternocleidomastoid muscle
b) Posteriorly: Anterior border of the trapezius muscle
c) Inferiorly: clavicle
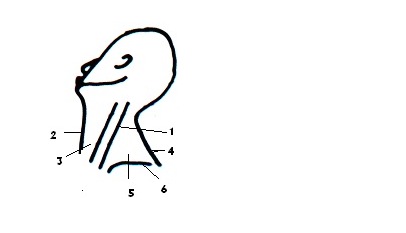
1) Sternocleidomastoid
2) Midline
3) Anterior triangle
4) Trapezius
5) Posterior Triangle
6) Clavicle
Lumps in the anterior triangle: node, thyroid lump, thyroglossal cyst and branchial cyst
Lumps in the posterior triangle: node, cystic hygroma and neuroma
Summary
1) The majority of neck lumps are reactive lymph nodes and usually settle once the primary source of infection is treated
2) Smoking and alcohol consumption are significant risk factors in cancers of the head and neck.
3) Patients with symptoms such as dysphagia, dysphonia, dyspnoea and weight loss need referral for an ENT assessment.
4) A persistent lymph node in the neck (> 6 weeks) needs referral for assessment of the upper aerodigestive tract.
References
1) Shared care for ENT (1997) by Chris Milford and Aled Rowlands
2) Expert Guide to Otolaryngology: Karen H.Calhoun, David E. Eibling and Mark K. Wax.
3) Key topics in Otolaryngology (second edition) N J Roland, R.D.R.Mc Rae and A.W. Mc Combe.
Authors
1) Mr.V.Visvanathan MRCS (Edin), DOHNS
Senior House Officer in Surgery
West Midlands
Birmingham
B29 6JD
2) Tiera Galm MRCS, DOHNS
Specialist Registrar in ENT
Stafford General Hospital
Stafford
ST16 3RS
Fublished May 2007
Copyright Priory Lodge Education Ltd. 2007
Click
on these links to visit our Journals:
Psychiatry
On-Line
Dentistry On-Line | Vet
On-Line | Chest Medicine
On-Line
GP
On-Line | Pharmacy
On-Line | Anaesthesia
On-Line | Medicine
On-Line
Family Medical
Practice On-Line
Home • Journals • Search • Rules for Authors • Submit a Paper • Sponsor us
All pages in this site copyright ©Priory Lodge Education Ltd 1994-


