Browse through our Medical Journals...
Deliberate Self-Harm: the breadth and scope.

Deliberate Self Harm - DSH
Introduction
What is deliberate self-harm (DSH)?
Deliberate self harm (DSH) is the term sometimes used for self injury or even self mutilation. the term itself is controversial and people who self harm sometimes dislike the adjective 'deliberate', but this is there to distinguish the conscious and voluntary act from the accidental self harm. Some people who self harm would argue with the notion that the act is conscious or voluntary however.
If self-harm it is defined in terms of a conscious act by a person that causes themselves harm then this definition may encompass a wide variety of behaviours that do not immediately suggest psychiatric disorder. For instance is smoking a cigarette DSH? Smoking a cigarette is a conscious action, which most people now know, is harmful. Cigarette smokers are not however currently thought of as psychiatrically ill.
If we are to understand why some harmful acts are considered to be DSH and why some others are not currently seen as DSH we must try and understand a complex area of behaviours which are subject to judgments influenced by training, experience, culture, religion, art and fashion.
I was trained in psychiatry in the 1980s and 1990s and have worked as a consultant psychiatrist in student health, occupational health and female secure services. I was a senior registrar in one of Europe’s busiest Accident & Emergency Departments so I have some twenty years’ experience of working with people who DSH. I still find the area a puzzle and a challenge, and it still causes me anxiety. I come from a discipline that has distinct views regarding DSH that recognizes such acts as repeated self-cutting or deliberate overdoses as self-harm, that is to say pathological. There are less certain areas for psychiatry – anorexia nervosa is not traditionally put under the umbrella of DSH, not is substance abuse, but there are underlying themes and similarities that are undeniable.
The definition is important, because our research depends upon it and if the definition is incorrect or has false assumptions embedded within it, then we will struggle to find solutions.
 |
 |
 |
 |
| DSH or religion? | DSH or art? | DSH or protest? | DSH or fashion? |
There are contentious areas in religion, art, politial protest and fashion that involve acts of self harm, but the motives behind the acts often lead some clinicians to deny that they are pathological in the sense of psychopatholog. What do you think?
Even today research clumps some acts 'legitimately defined' as DSH together e.g. self poisoning and self cutting - that may have very different purposes for the individual – and do not include other acts of DSH or do not include acts of DSH that do not present to doctors – so the gaps in our research knowledge are huge.
Population surveys have suggested that there is an apparent explosion of DSH behaviours in the urban young in the developed world – and we struggle to grasp the meaning of these – does this represent an increased incidence of DSH - a reflection of an overcrowded and more stressed society? Or is it that we have not previously tapped into or acknowledged some behaviours which were hitherto just not presenting to health services?
Traditionally psychiatrists have assessed DSH in terms of the psychiatric disorders usually associated with suicidal behaviours -depression, schizophrenia, borderline personality disorder, and substance misuse. Does the self-cutting adolescent really have a psychiatric disorder or should we view this behaviour as a ‘variant of normal’, given its apparent prevalence? If the individual does not seek or wish professional help what should services do? The attitudes of staff are crucial in determining the service response, and long exposure of staff to people who DSH may breed cynicism and minimization of the associated risks. As I will show current research suggests that repeated DSH is associated with eventual suicide and thus we do require some co-ordinated and evidence based response that is neither ‘psychiatric overkill’ nor a complacent denial of service based on pejorative labels such as ‘personality disorder’.
Demographics
All age groups can present with DSH. The prevalence of repeated DSH is higher in adolescents than in adults however (Hjelmeland & Groholt, 2005). Evans et al (2005) surveyed 6020 15-16 year-old school pupils with an anonymous questionnaire and adolescents with one or more episodes of DSH in the previous year were more likely to identify themselves as having serious problems than other adolescents. Adolescents with DSH were most likely to feel the need for help but not try to get any; they were less able to talk to family members and teachers and had fewer categories of people who they were able to talk to. This fits in with other groups observations regarding problem solving skills in repeated self harmers (see Management section).
An Australian study by De Leo and Heller (2004) looked at over 3000 schoolchildren in years 10 and 11. 233 students (6.2%) met the criteria for DSH in the previous 12 months, with DSH more common in females than males (OR, 7.5; 95% CI, 5.1-10.9). The main methods were self-cutting (138 respondents; 59.2%) and overdosing with medication (69 respondents; 29.6%). Factors associated with DSH included similar behaviours in friends or family, coping by self-blame, and self-prescribing of medications. Most self-harmers did not seek help before or after their most recent action, with those who did primarily consulting friends.
Ruths et al (2005) performed a retrospective analysis of DSH in the aged in North London and found that most cases involved self poisoning (82%) and that women, widows and the physically ill were proportionately over-represented vis-a-vis the general population.
Most acts of DSH, particularly in the young, may never come to the attention of a health professional (De Leo and Heller (2004). This is in the nature of what may be a secret and maladaptive coping behaviour. This may have various implications – not the least being that professionals develop a distorted view of the picture and that the research they in turn conduct may address only a fraction of the issue.
Much of the research considered here is hospital based and looks at issues of mortality (deaths) rather than morbidity (suffering) - Poustie & Neville (2004) considered the area of primary care and in an exploratory study used primary care team members to record all DSH episodes presenting over six months and their subsequent pattern of care over the next 12 months. Twenty five patients aged between 15 and 44 (19 females) presented at the practice during the six-month period. Fifteen had taken an overdose, nine had self-cut, and one case involved self-stabbing. Repeated DSH was the norm and an association with and substance misuse was almost universal. All patients were still alive after 12 months. Of the 13 patients initially in contact with secondary care services, only one established ongoing care. They concluded that the DSH patients had very high use of GP services, often in a chaotic manner. They recommended long-term management strategies from within primary care.
Deliberate self-harm (DSH) is a significant public health problem, representing a major burden in terms of morbidity for individuals and the health service. There are clinical guidelines for good practice in the short-term hospital management of DSH, but for medium and long term management there is great variability in provided services (Sinclair et al, 2006).
Outcome of DSH
Hawton et al (2006) studied national death registries to help follow up 11,583 adults who had presented to hospital with DSH over a 20year period. The number of deaths (1,185, 10.2%) was 2.2 times the expected number, the excess being significantly greater in males than females. Suicides were 17 times more frequent than expected and undetermined causes of death and accidental poisonings 15 times more frequent. DSH patients were found to be at increased risk of dying from a wide range of other causes. This could be because they had physical illnesses which precipitated the DSH or they are coincident lifestyle factors associated with DSH and physical disorders e.g. smoking or alcohol misuse and social disadvantage.
Hawton & Harriss (2006) conducted a 20 year follow-up of 730 consecutive patients (459 females and 271 males) aged 60 years and over who presented to a general hospital after DSH. Most of these (86%) were overdoses and initial suicidal intent was deemed high. Episodes of DSH were precipitated by physical illness (46.1%), social isolation (33.5%), relationship problems with family (29.4%) or partner (25.9%), and bereavement or loss (16.7%). 15 % of episodes were followed by further DSH. There were 30 suicides and open verdicts, which were 49 times and 33 times more frequent respectively than expected
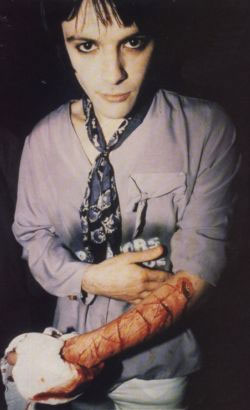 |
"When I cut myself I feel so much better, all the little things that might have been annoying me suddenly seem so trivial because I'm concentrating on the pain. I'm not a person who can scream and shout so this is my only outlet. It's all done very logically." Reported Comment of Richie James of the Manic Street Preachers who carved '4 real' on his arm when challenged by a journalist to prove his self harming was not a pose. Richie James sadly went missing in 1995 and his car was found abandoned near the Clifton Suspension Bridge, a notorious suicide spot. |
Although suicide is highly associated with DSH, and that suicidal intent at the time of deliberate self-harm is associated with a risk of future suicide the science of precisely predicting which DSH patient will eventually kill themselves is difficult. Hawton (2005) looked at the predictive value of the Beck Suicidal Intent Scale. He studied clinical and demographic data on 4156 DSH patients presenting to hospital between 1993 and 1997. Follow-up information on eventual suicide was available for 2489 patients (mean follow-up 5.2 years). Thirty males (2.9%) and 24 females (1.7%) died by suicide. The positive predictive value of the Beck Suicidal Intent Scale (SIS) was low (4%).
Zahl and Hawton (2004) investigated the long-term risk of suicide associated with repetition of DSH. They looked at details of the 11 583 people who presented with DSH to the general hospital in Oxford between 1978 and 1997. Thirty-nine per cent of patients repeated the DSH. They were found to be at greater relative risk of suicide than the single-episode DSH group (2.24; 95% CI 1.77-2.84).
Other risk factors
In a Swedish study of girls aged 12-19 years hospitalisation for DSH was associated with female-headed families, social welfare recipients and low-income families (Reimers & Laflamme, 2006).
In schizophrenia DSH behaviour is thought of as a strong predictor of suicide. Haw et al (2005) looked at additional risk factors and found that in these DSH patients with schizophrenia suicide was also associated with past or recent suicidal ideation, previous DSH, past depressive episode, drug abuse or dependence, and higher mean number of psychiatric admissions. Rather counter-intuitively unemployment in this study was associated with a reduced risk of suicide.
Hawton et al (2002) found a family history of suicide in 36% of DSH presenters, usually the suicidal behaviour reported was in the mother rather than the father. Amongst these patients there were higher state anger scores.
Management
Sinclair et al (2006) commented that further research is needed to evaluate the impact of different styles of service provision on outcome.
Much may depend on the nature of the DSH – e.g. the suicidal intent, presence or absence of depression and the repetitive nature of some DSH as a maladaptive coping behaviour. The correct management of the high suicidal intent person with affective disorder may be very different to the successful management of a repeated DSH.
One possible impediment to developing a coherent management strategy may be the attitudes and skills of staff themselves. Friedman et al (2006) looked at the attitudes of accident and emergency (A&E) staff towards patients who self-harm through laceration. Although staff believed that self-laceration was an important problem they felt unskilled in managing patients. They were unaware of the high risk of suicide statistically, but had received little training in the area. Staff who had longer experience and less training were less sympathetic, and this may impact on management of self-cutters. In a comparable study looking at staff actually working with adolescents some gaps in knowledge about DSH were found by Crawford et al (2003). For instance they found staff unaware that homosexual young men and those who had been sexually abused are at greater risk of DSH, and one third of the staff was unaware that adolescents who self-harm are at increased risk of suicide. Staff who felt more effective felt less negative towards this group of patients, arguing perhaps the need for enhanced training in effective techniques. Indeed 43% wanted more training.
In recent years the observations that psychological denial and avoidance of problems may underlie maladaptive coping mechanisms such as DSH has led to the investigation of whether people with DSH have poor problem solving skills leading to clinical spin offs in terms of teaching problem solving skills as an intervention. McAuliffe et al (2006) wrote up part of the WHO/EURO Multicentre Study on Suicidal Behaviour. In this 836 medically treated DSH patients (59% repeaters) from 12 European regions were interviewed approximately 1 year after their index episode. They looked at problem solving and found five dimensions: Active Handling, Passive-Avoidance, Problem Sharing, Palliative Reactions and Negative Expression. Of these Passive-Avoidance -(a pre-occupation with problems, feeling unable to do anything, worrying about the past and taking a gloomy view of the situation, a greater likelihood of giving in so as to avoid difficult situations, the tendency to resign oneself to the situation, and to try to avoid problems) was the problem-solving dimension most strongly associated with repetition of DSH. They advocated intensive therapeutic input with focus on problem solving and also emphasized the value of follow-up for those with repeated DSH.
Managing children who do not come forward for help is intrinsically difficult and De Leo and Heller (2004) suggested awareness programs to encourage teenagers who DSH to come forward for appropriate help. Teenagers who do present to A&E though, depending on where they live, may not receive follow up care (McAlaney et al 2004). Where specialist DSH services are offered to teenagers (Haw et al, 2003) they are generally acceptable and 2/3 of teenagers take up the offer of care.
Conclusions
• DSH is a complex area and what is deemed pathological self injury is subject to change over time and with culture and religion.
• Repeated DSH is more associated with eventual completed suicide than a single episode of DSH.
• The association of DSH with suicide means that ethically mental health services should adopt an evidence-based and longer-term strategy to positively and sympathetically help people with DSH problems.
• Alternative methods of communication and problem solving should be advocated and taught, particularly in adolescent settings.
• A holistic approach seeing the individual as a whole rather than a personality disorder would be preferable.
• Staff training is desirable to give information about DSH and the associated risks – to take it seriously - and create a positive attitude in staff and patients that change can occur and those solutions to problems can be found.
• Concomitant illnesses such as depression, PTSD or bipolar affective disorder must be vigorously treated.
• It is best not to make unjustified assumptions about what DSH is or what its psychological purpose for the individual is.
• DSH can occur in males as well as females and can occur in any age group.
Dr Ben Green, MRCPsych, FHEA,
Consultant Psychiatrist Cheadle Royal Hospital and Honorary Senior Lecturer, University of Liverpool, UK.
References
Crawford, Tanya. Geraghty, Wendy. Street, Karen. Simonoff, Emily. Staff knowledge and attitudes towards deliberate self-harm in adolescents. Journal of Adolescence. 26(5):623-33, 2003 Oct.
De Leo, Diego. Heller, Travis S. Who are the kids who self-harm? An Australian self-report school survey. Medical Journal of Australia. 181(3):140-4, 2004 Aug 2.
Evans, Emma. Hawton, Keith. Rodham, Karen. In what ways are adolescents who engage in self-harm or experience thoughts of self-harm different in terms of help-seeking, communication and coping strategies? Journal of Adolescence. 28(4):573-87, 2005 Aug.
Friedman, Trevor. Newton, Charles. Coggan, Christine. Hooley, Samantha. Patel, Rekha. Pickard, Matthew. Mitchell, Alex J. Predictors of A&E staff attitudes to self-harm patients who use self-laceration: influence of previous training and experience. Journal of Psychosomatic Research. 60(3):273-7, 2006 Mar.
Haw, Camilla. Hawton, Keith. Whitehead, Linda. Houston, Kelly. Townsend, Ellen. Assessment and aftercare for deliberate self-harm patients provided by a general hospital psychiatric service. Crisis: Journal of Crisis Intervention & Suicide. 24(4):145-50, 2003.
Haw, Camilla. Hawton, Keith. Sutton, Lesley. Sinclair, Julia. Deeks, Jonathan. Schizophrenia and deliberate self-harm: a systematic review of risk factors. Suicide & Life-Threatening Behavior. 35(1):50-62, 2005 Feb.
Hawton, Keith. Haw, Camilla. Houston, Kelly. Townsend, Ellen. Family history of suicidal behaviour: prevalence and significance in deliberate self-harm patients. Acta Psychiatrica Scandinavica. 106(5):387-93, 2002 Nov.
Hawton, K. Suicidal intent in deliberate self-harm and the risk of suicide: the predictive power of the Suicide Intent Scale. Journal of Affective Disorders. 86(2-3):225-33, 2005 Jun.
Hawton, K. Harriss, L. Zahl, D. Deaths from all causes in a long-term follow-up study of 11,583 deliberate self-harm patients. Psychological Medicine. 36(3):397-405, 2006 Mar.
Hawton, Keith. Harriss, Louise Deliberate self-harm in people aged 60 years and over: characteristics and outcome of a 20-year cohort. International Journal of Geriatric Psychiatry. 21(6):572-81, 2006 Jun.
Hjelmeland, H. Groholt, B. A comparative study of young and adult deliberate self-harm patients. Crisis: Journal of Crisis Intervention & Suicide. 26(2):64-72, 2005.
McAlaney, John. Fyfe, Margo. Dale, Maria. A specialist adolescent self-harm service. Nursing Standard. 18(17):33-8, 2004 Jan 7-13.
McAuliffe, Carmel. Corcoran, Paul. Keeley, Helen S. Arensman, Ella. Bille-Brahe, Unni. De Leo, Diego. Fekete, Sandor. Hawton, Keith. Hjelmeland, Heidi. Kelleher, Margaret. Kerkhof, Ad J F M. Lonnqvist, Jouko. Michel, Konrad. Salander-Renberg, Ellinor. Schmidtke, Armin. Van Heeringen, Kees. Wasserman, Danuta. Problem-solving ability and repetition of deliberate self-harm: a multicentre study. Psychological Medicine. 36(1):45-55, 2006 Jan.
Poustie, Anne. Neville, Ron G. Deliberate self-harm cases: a primary care perspective. Nursing Standard. 18(48):33-6, 2004 Aug 11-17.
Reimers, A. Laflamme, L. The neighbourhood socio-demographic context of teenage girls' deliberate self-harm. International Journal of Injury Control & Safety Promotion. 13(4):227-33, 2006 Dec.
Ruths, Florian Alexander. Tobiansky, Robert Ian. Blanchard, Martin. Deliberate self-harm (DSH) among older people: a retrospective study in Barnet, North London.International Journal of Geriatric Psychiatry. 20(2):106-12, 2005 Feb.
Sinclair, Julia M A. Gray, Alastair. Hawton, Keith. Systematic review of resource utilization in the hospital management of deliberate self-harm. Psychological Medicine. 36(12):1681-93, 2006 Dec
Zahl, Daniel Louis. Hawton, Keith. Repetition of deliberate self-harm and subsequent suicide risk: long-term follow-up study of 11,583 patients. British Journal of Psychiatry. 185:70-5, 2004 Jul.
First Published April 19th 2007
Copyright Priory Lodge Education Limited 2007
This lecture was given at Manchester Conference Centre on 19th April 2007.
Click
on these links to visit our Journals:
Psychiatry
On-Line
Dentistry On-Line | Vet
On-Line | Chest Medicine
On-Line
GP
On-Line | Pharmacy
On-Line | Anaesthesia
On-Line | Medicine
On-Line
Family Medical
Practice On-Line
Home • Journals • Search • Rules for Authors • Submit a Paper • Sponsor us
All pages in this site copyright ©Priory Lodge Education Ltd 1994-


