Browse through our Journals...
Behavioral Disorders in Human Immunodeficiency Virus (HIV)
Infected Adolescents in the Age Group 12-16 years in India
Tanushree Banerjee, M.Phil, Department of Statistics, University of Delhi,
India.
Tripti Pensi, MD, Department of Pediatrics, Dr. Ram Manohar Lohia
Hospital, New Delhi, India. Gurprit Grover, PhD., Department of Statistics, University of Delhi, India.
Summary
International studies and clinical reports have suggested that HIV-positive children and adolescents are at risk for behavioral problems. The transition of HIV from an acute, lethal disease to a sub acute, chronic disease has enormous implications for the neurocognitive and psychosocial development of children and families. A prospective study was planned to examine the unique and combined influences of HIV and socio-demographic characteristics on behavior of 441 children (140 infected and 301 age and income matched controls) in 4-16 years of age for which random sampling approach was used. Child Behavior Check List was utilized in assessing behavior patterns in each child. Multivariate analyses comparing children and adolescents with HIV infection with their uninfected peers from similar backgrounds showed more subjective distress in the HIV-infected children. 80.7% HIV-infected children reported behavioral problems by their primary caregivers as compared to 18.3% of healthy control group. Psychiatric behavior in HIV-infected children as risk factor for HIV was also identified in significant proportion (p<0.0001) in our study. By the behavioral analysis, psycho medical team can examine the extent to which psychosocial and demographic factors are involved in causation and exacerbation of behavior problems in HIV-infected children.
KEYWORDS:
CBCL; children; HIV; psychiatric disorders; 12-16 years.
1. Introduction
Human immunodeficiency virus (HIV) is a global health threat of significance to child and adolescent psychology and psychiatry. Rapidly increasing incidence of pediatric acquired immunodeficiency syndrome (AIDS) and HIV documents the consequences of the epidemic in the care and development of children and youth infected by HIV and in the change of risk behavior among both the infected and the affected (Brown and Lourie, 2000).
Although clinical reports suggest that adolescents with HIV infection are more likely to report limitations that are behavioral and emotional rather than physical (Remafedi, 1998), there are few research studies which have focused on the complexity of their impairment. Moreover, the prevalence rates of psychiatric disorders in HIV-infected children and adolescents are unknown.
Understanding the cause of behavioral problems in HIV-infected children and adolescents is critical for improving their mental health and quality of life. Also, given the evidence that mental health problems are associated with poor medication adherence even in adults, improving the mental health of HIV-infected children and adolescents may have an impact on their overall growth and development and the quality of life of the individual and the entire family (Mellins et al., 1999; Philadelphia, Rabkin and Chesney, 1998).
This is a study to focus exclusively on the estimation of psychosocial development of HIV-infected and effected adolescents in the age-group of 12-16 years. It is also planned to study the combined influences of HIV and socio-demographic characteristics on behavior of adolescents. This study further aims to provide empirical information about the prevalence and correlates of psychological problems in a hospital based sample of HIV-infected adolescents with the goal of broadening the understanding of mental health needs in the present Indian context and highlighting key features that may be useful flags for focusing on families that may benefit from further evaluation and treatment.
The results of the study undertaken will help to formulate policy and programmes for the adolescents and their families affected with HIV/AIDS as investing in adolescents is must as they alone are the future of the country.
2. Methods and Aims
2.1 Study Population
A prospective study was carried out among the HIV-infected patients regularly attending the Pediatrics HIV outpatient clinic of the Dr. Ram Manohar Lohia (RML) Hospital, New Delhi between October 2005 and June 2006. A total of 170 children and adolescents accompanied by their caregivers were visiting the HIV outpatient clinic at RML Hospital during the study period. Eligibility criteria for the current study included the child to be within the age group of 4-16 years. Thus, 140 children were eligible; 18 children were ineligible because they were <4 years of age by June 2006. Of the potentially eligible children, 5 expired, 3 dropped out of the ARV treatment and 4 refused to be interviewed. At the time of enrollment, a group of healthy controls was considered to assess whether HIV-1 infection per se had any influence on the behavioral functioning of HIV-1 infected children and adolescents. The controls were age and income matched children with no known preexisting illness that might have interfered with the behavioral symptoms. We planned to enroll two potential controls of similar age for each patient attending the HIV clinic. Subsequent to obtaining informed consent 301 subjects were recruited as potential controls.
The present study was approved by the Ethics Committee of Dr. Ram Manohar Lohia Hospital, New Delhi. A signed consent form was obtained from the parents or caregivers before enrollment.
2.1.1 Procedures
All children and adolescents who were coming to the HIV pediatrics outpatient clinic received routine physical and HIV associated examinations throughout the course of the study. Relevant to this article, a behavioral functioning questionnaire was administered to the primary caregivers of each child by psychometricians or pediatric psychologists who completed centralized training in proper administration and scoring of this tool.
Data on demographics (e.g. primary language, maternal education, and child grade level), medical status, details of family composition and monthly household income were also collected from primary caregivers at the time of interview.
2.1.2 Instrument
The Child Behavior Check List (CBCL) (Achenbach and Edelbroch, 1983) is a well-standardized and widely used 118-item rating scale for the identification of behavioral and emotional problems in children observed by caregivers. It is a multi axial empirically based scales, normed by age and gender assess social competencies as well as behavior/emotional problems. Even though CBCL does not form a diagnosis, it is used as an outcome measure for assessment. CBCL consists of 2 parts: 20 social competence items and 118 behavior problem items.
In this study only the behavior problem items were considered which is of concern to parents and clinicians. Primary caregivers are asked to describe how much a particular behavior was characteristic of their child in the past 6 months, using a 3 point rating scale (“2” if the item is true, “1” if the item is somewhat true or “0” if the item is not true). Responses from the primary caregiver to the items yield raw and T scores for each total behavior problem score, based on age and gender normative data. Higher T scores on the CBCL reflect greater degrees of symptoms. The clinical range of behavioral problems should be concerned with children whose scores are above 97 percentile.
2.1.3 Definitions
Adolescent HIV infection was defined as per WHO classification 2006 (WHO Case Classification, 2006). HIV infection was confirmed by Elisa Test that detected the presence of antibodies to HIV in children above 18 months. Two tests were done 4-6 weeks apart using three different principals (ERS).
Primary caregiver was defined as the caregiver with the most responsibility for caring for the child.
The sample size for comparison between two proportions was calculated, with predicted behavioral problems in 25% of the HIV-affected group compared to 5% of the control group. To obtain a confidence level of 95% and a power of 90% when comparing these two proportions, atleast 40 children had to be recruited into each group. The data were analyzed by using the SPSS 13.0 program. Correlation analyses were used to provide an initial assessment of the relations between the demographic parameters and HIV infection. Comparison of baseline demographic and clinical data was made by means of the Student’s t-test for continuous variables, and Chi-square test or Fisher’s exact test for categorical variables. A p-value of less than 0.05 was considered statistically significant. A stepwise discriminant analysis was performed over the demographic and other variables to select a best subset of predictor variables. Stepwise discriminant analysis is a multivariate statistical procedure that uses a set of explanatory variables to classify patients into different subgroups and allows the construction of a new variable namely, the predictive score. This score maximizes the ratio of the variability between the groups to the variability within the groups and therefore patients of different groups have score values as different as possible. Stepwise discriminant analysis was conducted over the behavioral clusters gender wise in the age group 12-16 years.
Multiple regression analysis was performed on the result of discriminant analysis on the predictor variables to examine the association of these variables with the T score obtained on the 118 behavioral traits. Regression analysis was also conducted to study the association of the predictor variables with the dominant behavioral clusters obtained gender wise in the age group 12-16 years by multivariate discriminant analysis.
3. Results
| Table 1: Demographics and Other Characteristics of the HIV-Infected Children and the Healthy Control Group. | |||
Predictors |
Cases (n=140) |
Control subjects (n=301) |
Statistical analyses by T-test |
T Score |
68.44 |
52.55 |
15.015 (0.001) |
Weight |
18.71 |
26.96 |
-10.933 (0.001) |
Number of times residence changed |
0.66 |
1.52 |
-6.182 (0.001) |
Number of times school changed |
0.39 |
1.43 |
-9.495 (0.001) |
Father’s Age |
35.41 |
40.56 |
-8.791 (0.001) |
Mother’s Age |
30.88 |
35.86 |
-9.152 (0.001) |
Table 1 summarizes the sociodemographic characteristics of the study population. Subjects and controls were demographically matched in terms of age and monthly income of the family. Demographic factors associated with the HIV infection were explored in our observed sample through correlation analyses. A series of Pearson correlation coefficients gave an initial assessment of the hypothesized relations between demographic parameters and HIV infection. The family environment, separation of the child from parents, rivalry between siblings and level of maternal education were not found to significantly relate to HIV infection. The death of father, weight of the child, death of mother, mother’s age and the remaining variables were examined as possible correlates of HIV infection. The factor viz. lack of father was examined to be highly correlated with the HIV infection (r = 0.565, p<0.01) which was followed by weight of the child (r = 0.463, p<0.01) and death of the mother (r = 0.431, p<0.01). To test our hypothesis of group differences on measures of demographic characteristics, we performed t-test for continuous variables and chi square test or Fisher’s exact test for categorical variables. Univariate analysis of the 17 predictor variables revealed that the rivalry between siblings and separation of the child from parents was insignificant in the two groups (χ2= 0.450, p=0.502) & (χ2= 1.913, p=0.167) respectively while all the other predictor variables showed significant difference in the two groups.
Table 2: Standardized Discriminant Coefficients of the Predominant Predictors in Discriminant
Analysis.
Step |
Variables |
Standardized Coefficient |
Wilks' Lambda |
P Value |
1 |
Weight |
.338 |
.747 |
.000 |
2 |
Death of father |
.539 |
.598 |
.000 |
3 |
Academic Performance |
-.422 |
.529 |
.000 |
4 |
Physical Ability |
-.277 |
.504 |
.000 |
5 |
Level of paternal education |
.211 |
.485 |
.000 |
6 |
Death of mother |
.244 |
.469 |
.000 |
7 |
Family Environment |
-.237 |
.458 |
.000 |
8 |
Number of times residence changed |
.200 |
.448 |
.000 |
9 |
Number of siblings |
-.217 |
.439 |
.000 |
10 |
Mother’s Age |
.230 |
.429 |
.000 |
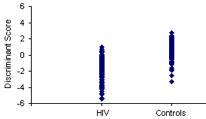
Figure 1 Values of a discriminant score in 140 HIV-infected children
and 301 healthy controls.
3.1 Multivariate Stepwise Discriminant Analyses. Multivariate stepwise discriminant analysis showed a significant discriminant function (canonical correlation r = 0.756; Wilk’s Lambda = 0.429; χ² = 337.956; df 10; p < 0.001) for the predictor variables weight, academic performance, physical ability, level of paternal education, age of mother, death of father, death of mother, total number of siblings, family environment and the number of times school has been changed. The variables with the largest influence on the discriminant function were the death of father followed by the academic performance of the child. Although the discriminant function analysis (DFA) selected a number of significant variables, the amount of variance explained by the function is about 57%. Further, it was observed that 82.9% of the HIV cases (sensitivity) and 96% of the healthy controls (specificity) were classified correctly in their respective categories, with an overall correct classification of 92.5%.
Table 3: Dominant Behavioral Clusters Genderwise in the Age Group 12-16 years
Step |
Variables |
Standardized Coefficient |
Wilks' Lambda |
P Value |
Boys |
||||
1 |
Somatic Complaints |
.671 |
.571 |
.000 |
2 |
Obsessive Compulsive |
.501 |
.516 |
.000 |
Girls |
||||
1 |
Somatic Complaints |
1.000 |
.196 |
.000 |
Figure 2 Values of a discriminant score in 13 HIV-infected children and 30 healthy controls
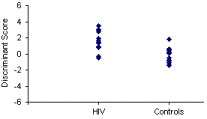
Figure 3 Values of a discriminant score in 4 HIV-
infected children and 30 healthy controls. infected children and 17 healthy controls.
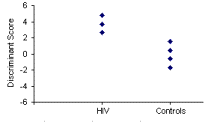
3.2 Stepwise Discriminant Analysis in the Age Group 12-16 years. Multivariate stepwise discriminant analysis revealed a significant discriminant function (canonical correlation r = 0.696, Wilk’s Lambda = 0.516, χ² = 26.490, df 2, P < 0.0001; canonical correlation r = 0.897, Wilk’s Lambda = 0.196, χ² = 30.167, df 1, P < 0.0001) for the nine behavioral clusters in boys and eight behavioral clusters in girls respectively in the age group 12-16 years. Analyses of each item evaluated by the CBCL in case of boys showed that HIV-infected children differed significantly from the control children as regards somatic complaints, schizoid, uncommunicative problems, obsessive compulsive disorders and factors related to immaturity, aggression and hyperactive behaviors (p<0.0001). No significant differences between the groups were observed as regards hostile withdrawal and delinquent issues (p>0.05). In case of girls significant differences between the groups were observed in factors related to somatic complaints, depressed withdrawal, immature and aggressive behaviors (p<0.001) while factors related to anxious obsessive, schizoid, delinquent and cruel behavioral symptoms did not show any significant differences between the groups. Inclusion of nine behavioral clusters in boys and eight behavioral clusters in girls by means of a stepwise discriminant analysis resulted in two main behavioral symptoms of somatic complaints and obsessive compulsive disorders in boys while only one symptom was observed in case of girls’ viz. somatic complaints (Table 3). The amount of variability in the behavioral symptoms as explained by the discriminant function in boys was about 48% whereas it was approximately 80% in girls. Discriminant analysis resulted in a discriminant score (allocation index) composed of these two variables in boys while in girls discriminant score was composed of a single variable. The discriminant score resulted in an overall correct classification of 86% with 10 of 13 HIV-infected cases being allocated to the HIV group (positive discriminant score) and 27 of 30 healthy controls to the healthy control group (negative discriminant score) in boys. Figure 2 shows the discriminant scores of the 43 subjects. Furthermore, in girls 100% of HIV-infected cases (sensitivity) and 94.1% of control group (specificity) were correctly classified with an overall correct classification of 95.2%. Figure 3 shows the discriminant scores of the 21 subjects.
Table 4: Multiple Regression Prediction of factors in CBCL scores for HIV-Infected Children and the Healthy Control Group (n=301)
Step |
Independent Variable |
R2 |
R2 change |
F change |
β |
1 |
HIV Infection |
.350 |
.350 |
220.852 |
-17.159* |
2 |
Family Environment |
.357 |
.007 |
4.341 |
4.101* |
F(2,409) for entire model = 113.497, p<0.0001
*p < 0.05
3.3 Multiple Regression Analyses. We conducted stepwise multiple regression analysis to test the factors having an independent effect on the total score. Specifically, guided by the result of discriminant analysis on the predictor variables, we entered variables in the following order: HIV infection, weight, number of times residence has been changed by the child, death of father, death of mother, mother’s age, total number of siblings, physical ability of the child, family environment, level of paternal education and the academic performance. The overall R2 when all variables hypothesized as significantly contributing to children’s T score were considered was significant, F (2,409) = 113.497, p<0.001, accounting for 36% of the variance (Table 4). Stepwise multiple regression analysis revealed that 2 factors viz. HIV infection and family environment of the child significantly contributed to the variance in children’s T score (β = -17.159, p< 0.001) and (β = 4.101, p< 0.05) respectively. No other factor made significant contribution to the variance in children’s T score. The tolerance for HIV infection was 0.860 thus, its R2 with the other ten independent variables was 0.14 (only 14% of the variability of HIV infection was explained by the other predictors). Furthermore, tolerance for the predictor variable family environment was again 0.860 which revealed that 14% of the variability of this variable was explained by the other ten predictors.
Table 5: Factors Associated with the CBCL Dominant Cluster Score in Boys in the Age
Group 12-16 years
Step |
Independent Variable |
R2 |
R2 change |
F change |
β |
Somatic Complaints Cluster |
|||||
1 |
HIV Infection |
.542 |
.542 |
42.532 |
-5.270* |
2 |
Mother’s Age |
.624 |
.083 |
7.684 |
.173** |
F(2,35) for entire model = 29.057, p<0.001 *p < 0.001; **p < 0.01 |
|||||
Obsessive Compulsive Cluster |
|||||
1 |
HIV Infection |
.348 |
.348 |
19.235 |
-3.300* |
2 |
Death of Mother |
.415 |
.067 |
4.012 |
-3.833 |
F(2,35) for entire model = 12.428, p<0.001 *p < 0.005 |
|||||
3.4 CBCL Behavioral Clusters in Boys in the Age Group 12-16 years. The demographic predictors as revealed by discriminant analysis and the HIV infection were entered into a regression equation predicting the predominant behavioral clusters as seen before in boys in the age group 12-16 years (Table 5). The overall R2 when all variables hypothesized as significantly contributing to children’s T score in the behavioral problems of somatic complaints and obsessive compulsive disorders were considered was significant, F (2,35) = 29.057, p<0.001 and F (2,35) = 12.428, p<0.001, accounting for approximately 62% of the variability in the somatic complaints group and 42% of the variance in the obsessive compulsive disorder cluster. Stepwise multiple regression analysis revealed that HIV infection and age of mother significantly contributed to the variance in the psychosocial symptom of somatic complaints (β = -5.270, p< 0.001) and (β = .173, p< 0.01) respectively while HIV infection and death of mother significantly contributed in the obsessive compulsive disorder symptom (β = -3.300, p< 0.005) and (β = -3.833, p< 0.005) respectively. The tolerance for HIV infection and family environment in the factor associated with somatic complaints was 0.701 and 0.701 respectively which accounted for 30% of the variability in HIV infection and family environment by the other predictors whereas the tolerance for HIV infection and death of mother in the factor associated with obsessive compulsive disorder was 0.792 and 0.792 respectively which accounted for approximately 21% of the variability in these variables by the other predictors.
Table 6: Factors Associated with the CBCL Dominant Cluster Score in Girls in the Age
Group 12-16 years
Step |
Independent Variable |
R2 |
R2 change |
F change |
β |
Somatic Complaints Cluster |
|||||
1 |
HIV Infection |
.804 |
.804 |
78.038 |
-4.544* |
F(1,19) for entire model = 78.038, p<0.001 *p < 0.001 |
|||||
3.5 CBCL Behavioral Clusters in Girls in the Age Group 12-16 years. The demographic predictors as revealed by discriminant analysis and the HIV infection were entered into a regression equation predicting the predominant behavioral clusters as seen before in girls in the age group 12-16 years (Table 6). The overall R2 when all variables hypothesized as significantly contributing to children’s T score in the behavioral problems of somatic complaints were considered was significant, F (1,19) = 78.038, p<0.001, accounting for approximately 80% of the variability in the somatic complaints group. Stepwise multiple regression analysis revealed that the HIV infection accounted for significant increment in the variance in the psychosocial symptom of somatic complaints (β = -4.544, p< 0.001). No other factor was a significant predictor of the somatic complaints symptom. The tolerance for the HIV infection in the behavioral symptom of somatic complaints revealed that the variability of HIV infection could not be explained by any other predictor variable.
4. Discussion
113 children (80.7%) with HIV infection and 55 (18.3%) in the healthy control group were reported as having behavioral problems by their primary caregivers, whereas only 27 (19.3%) HIV cases and 246 (81.7%) control subjects had CBCL scores within the clinical range. Literature reveals that children and adolescents with HIV infection experience more subjective distress than their uninfected peers, including dysphoria, hopelessness, preoccupation with their illness, and poor body image. Some adolescents with HIV report more sexual risk-taking behavior and conduct or hyperactivity disorders (Brown and Lourie, 2000; Remafedi, 1998). The cultural context of HIV transmission is an important factor in the care of infected youth (Williams and Ponton, 1992). Despite this, little is known about the specific factors that predict psychological adjustment in these children and youth, or is it known how these children and families fare when compared to families of similar backgrounds. This study found that majority of the HIV-infected children and adolescents was experiencing significant behavioral disorders which are consistent with other studies that have shown that children with chronic illnesses are at risk for significant behavioral disorders (Wallander and Varni, 1998; Bose et al., 1994; Pao et al., 2000; Tardieu et al., 1995).
The etiology of behavioral abnormalities in HIV-infected children and adolescents is likely to be multifactorial, including factors such as prenatal drug exposure, difficult family environment, age of parents, level of parental education, absence of parent, changes in caregivers, nutrition and poverty (Nozyee, 2006). Information on majority of these factors was elicited and explored in this analysis. There was significant difference in the characteristic backgrounds including health of the child indicated by weight and the parent’s age. The mean weight and parents’ education was significantly lower among HIV-infected children and adolescents compared with the controls although the family income of the HIV-infected children and adolescents had been matched with that of the controls (Table 1). The univariate findings support the concept that socio-demographic factors such as difficult family environment, level of paternal education, level of maternal education, death of mother, and death of father were characteristics associated with HIV-infected children and adolescents. However, in our study, we failed to find an association between the factors viz. number of times residence and school changed and the HIV-infected group. In India, it has been observed that HIV infection is more prevalent among the poor people. The findings could reflect that majority of the families of the HIV-infected children and adolescents were dwelling in slums which they considered their permanent residence therefore did not move from one place to other. On the other hand families of the controls were mostly into transferable jobs thereby living in rented accommodations which gave them an opportunity to move from one location to another.
DFA reinforces the univariate findings that the demographic characteristics and the T score significantly differentiate the two groups (Figure 1). It was observed that two of the ten variables (death of father and academic performance) have relatively high standardized coefficients (Table 2). Thus it was seen that these two factors were the only discriminating points between the HIV and the healthy control groups. All other variables were of minor importance compared to these two factors although they made significant contributions in DFA.
Previous studies have found prevalence rates of various behavioral disorders, including attention-deficit/hyperactivity disorder (ADHD), to differ by gender (Szatmari, Offord and Boyle, 1989; Ross and Ross, 1982; Trites, 1979). However, the current analysis did not reflect any behavioral difference between boys and girls (RR= 1.113, 95% CI: 0.748-1.657, p>0.05).
Current analysis revealed that among boys in the age group 12-16 years the psychosocial symptoms of somatic complaints and obsessive compulsive disorders contributed significantly to the behavioral syndromes (p<0.0001) (Table 3). On the other hand behavioral symptoms in girls of 12-16 years were related only to the somatic complaints problem (p<0.001) (Table 3). No other behavioral syndrome was a significant predictor of the psychiatric disorders in girls in the age group 12-16 years (p>0.05).
Further analysis of the study revealed high rates of emotional and behavioral problems in HIV-infected children and adolescents compared with the healthy control group (p<0.0001) which correspond with previous studies (Esposito et al., 1999; Forehand et al., 1998). The strongest correlates of increased behavioral symptoms in this study consistently were HIV infection and the disturbed family environment of the child. On analyzing the predominant behavioral clusters gender wise in the age group 12-16 years of age, it was observed that in boys HIV infection was a major contributory factor towards behavioral disorders. The factors viz. mother’s age and lack of mother contributed towards the somatic complaints problem and obsessive compulsive disorder respectively along with the HIV infection (Table 5). It was noted that in girls HIV infection was the only contributory factor towards the behavioral disorders in the concerned age group (Table 6). However, previous studies of behavioral symptoms in HIV-1 infection in infants and school-age children have produced conflicting findings which have shown that high rates of behavioral problems in HIV infected infants and school-age children are not linked to the HIV disease (Mellins et al., 2003; Havens et al., 1994; Loveland et al., 1994; Whitt et al., 1993; Brouwers et al., 1992). This apparent discrepancy could be attributable to the inadequate control groups and sample sizes that have limited the ability of the investigators to consider multiple influences that place HIV-positive children at risk for poor behavioral outcomes. The present study revealed that in our sample of HIV infected children and adolescents and the healthy control group, HIV infection gave a good representation of all the variables considered for the contribution towards behavioral symptoms.
The result obtained from the present study reaffirms the need to acknowledge the crucial role of psychosocial support for HIV infected and affected adolescents. Adolescent-specific factors, such as cognitive immaturity and exploratory learning behavior as well as a variety of other factors that moderate sexual behavior, such as impulsivity, distress and adverse life experiences need to be targeted by intervention programs. The work of medical personnel and policy makers should be focused not only to prolong the HIV-infected adolescent’s life span but also to strive for a good quality of life of these individuals.
5. Conclusions
To summarize, a number of reports have suggested that HIV-infected children are at a high risk for behavioral problems. The results of our study demonstrate significant differences in behavioral outcomes, as assessed by the CBCL scores, between the HIV-infected children and adolescents and the healthy control group. To the extent that there is a high prevalence of behavioral problems among HIV-infected children and adolescents, our findings suggest that HIV infection along with disturbed family environment of the child is the underlying cause. A variety of stressors are experienced by the majority of HIV-infected and affected children in India, including trauma, number of hours spent by the parent with the child, HIV illness of the parent and familial mental illness in the home that may be contributors toward poor behavioral outcomes. Future studies are needed to further our understanding of how other environment and biological factors influence behavior in this population.
These findings reflect the need of psychosocial interventions on the psychological adjustment of children and adolescents with HIV, given the large number of children with HIV infection who were reporting significant behavioral problems. Future studies should seek to evaluate the efficacy of these interventions (e.g., support groups, individual and family therapy, case management, etc.) for children and families as they struggle to cope with this devastating disease. In addition, these findings also highlight the need for case management, social work, and mental health services to be available for at-risk families in the study, as many healthy children and adolescents exhibited significant levels of psychological distress and poor adjustment.
References
Achenbach, T.M. and Edelbrock, T. (1983) Manual for the Child Behavior Check List and Revised Child Behavior Profile. Burlington, VT: University of Vermont.
Bose, S., Moss, H.A., Brouwers, P., et al. (1994) Psychologic adjustment of HIV-infected school-age children, Developmental and Behavioral Pediatrics, 15, S26-S33.
Brouwers, P., Moss, H., Wolters, P., et al. (1992) Neurobehavioral typology of school-age children with symptomatic HIV disease, J Clin Exp Neuropsychol, 12, 113 (abstr).
Brown, L.K. and Lourie, K.J. (2000) Children and Adolescents Living with HIV and AIDS: A Review, J Child Psychol Psychiat, 41, 81-96.
Esposito, S., Musetti, L., Musetti, M.C., et al. (1999) Behavioral and psychological disorders in uninfected children aged 6 to 11 years born to human immunodeficiency virus-seropositive mothers, J Dev Behav Pediatr, 20, 411-417.
Forehand, R., Steele, R., Armistead, L., et al. (1998) The Family Health Project: Psychosocial adjustment of children whose mothers are HIV infected, J Consult Clin Psychol, 66, 513-520.
Havens, J., Whitaker, A., Feldman, J., et al. (1994) Psychiatric morbidity in school-age children with congenital HIV-infection: a pilot study, J Dev Behav Pediatr, 15, S18:S25.
Loveland, K.A., Stehbens, J., Contant, C., et al. (1994) Hemophilia growth and development study: baseline neurodevelopmental findings, J Pediatr Psychol, 19, 223-229.
Mellins, C.A., McCaskill, E., Havens, J., et al. Factors mediating medical adherence in HIV-infected mothers. Paper presented at the annual conference of the NIMH on “The Role of Families in Preventing and Adapting to HIV-infection and AIDS.” July 1999.
Mellins, C.A., Smith, R., O’Driscoll, P., et al. (2003) High rates of Behavioral Problems in Perinatally HIV-Infected Children are not linked to HIV Disease, Pediatrics, 111 (2), 384-393.
Nozyce, M.L., Lee, S.S., Wiznia, A., et al. (2006) A Behavioral and Cognitive Profile of Clinically Stable HIV-Infected Children, Pediatrics, 117 (3), 763-770.
Pao, M., Lyon, M., D’Angelo, L., et al. (2000) Psychiatric diagnoses in adolescents seropositive for the human immunodeficiency virus, Arch Pediatr Adolesc Med, 154, 240-244.
Philadelphia, P.A.., Rabkin, C. and Chesney, M.A. (1998) Adhering to complex regimens for HIV, GMHC Treat Iss., 12, 8-11.
Remafedi, G. (1998) The University of Minnesota Youth and AIDS Projects’ Adolescent Early Intervention Program, J Adolesc Health, 23, 115-121.
Ross, D.M. and Ross, S.A. (1982) Research, Theory and Action. NY: Wiley Press. New York.
Szatmari, P., Offord, D.R. and Boyle, M.H. (1989) Correlates, associated impairments and patterns of service utilization of children with attention deficit disorders: findings from the Ontario Child Health Study, J Child Psychol Psychiatry, 30, 205-217.
Tardieu, M., Mayaux, M.J., Seibel, N., et al. (1995) Cognitive assessment of school-age children infected with maternally transmitted human immunodeficiency virus type 1, J Pediatr, 126, 375-379.
Trites, R.L. (1979) Hyperactivity in Children: Etiology, Measurement and Treatment Implications. MD: University Park Press. Baltimore.
Wallander, J.L. and Varni, J.W. (1998) Effects of pediatric chronic physical disorders on child and family adjustment, Journal of Child Psychology and Psychiatry, 39, 29-46.
Whitt, J.K., Hooper, S.R., Tennison, M.B., et al. (1993) Neuropsychologic functioning of human immunodeficiency virus-infected children with hemophilia, J Pediatr, 122, 52-59.
Williams, R. and Ponton, L.E. (Eds.). (1992) Special issues on HIV-AIDS and adolescents, J Adolescence, 15, 335-483.
WHO Case Classification (2006).
(Available from http://www.who.int/hiv/pub/guidelines/casedefinitions/en/index.html.).
Corresponding Author:
Tanushree Banerjee
A-123 Vikaspuri
New Delhi-110018, India.
Tel. No.: 91-11-25545933, 91-11-25617422
First Published May 2007
Copyright © Priory Lodge Education Limited 2007
Presented abstract of the paper (CDC 1038) at XVI International AIDS
Conference; 13-18 August, 2006; Ontario; Toronto, Canada.
Click
on these links to visit our Journals:
Psychiatry
On-Line
Dentistry On-Line | Vet
On-Line | Chest Medicine
On-Line
GP
On-Line | Pharmacy
On-Line | Anaesthesia
On-Line | Medicine
On-Line
Family Medical
Practice On-Line
Home • Journals • Search • Rules for Authors • Submit a Paper • Sponsor us
All pages in this site copyright ©Priory Lodge Education Ltd 1994-


