Browse through our Journals...
The assessment and management of benzodiazepine misuse and dependence
Dr Kudlur Thyarappa Praveen MRCPsych
Specialty Registrar (Year 5)
BSDAS, Blackberry Centre,
Blackberry Hill hospital
Avon & Wiltshire Mental Health NHS trust
Bristol BS16 2EG
*Dr Sanju George MRCPsych
Consultant and Senior Research Fellow in Addiction Psychiatry
The Bridge Substance Misuse Clinic
Birmingham and Solihull Mental Health NHS Foundation Trust
Birmingham
B37 7UR
* Correspondence
ABSTRACT
Benzodiazepines are routinely prescribed in clinical practice for treatment of anxiety, insomnia, epilepsy and muscle spasms but their misuse and dependence is common. Indicators of benzodiazepine misuse are over reliance on regular prescriptions, dosage escalation, unsuccessful attempts to cut-down or stop drug use and high anxiety levels. This article discusses the assessment and management of benzodiazepine misuse and dependence.
Introduction
Benzodiazepines are a group of drugs used in the treatment of anxiety, insomnia, seizures and muscle spasms but patients often misuse them for both medical and nonmedical reasons. Dependence to these drugs following repeated use has been noted for over two decades. More often, its misuse and dependence develop in those prescribed these drugs for medical reasons - referred to as ‘therapeutic dose dependence’. Another group who are benzodiazepine dependent are poly drug users, and they seek medical help with established dependence. In this paper, we will discuss the assessment and management of benzodiazepine misuse and dependence in the former group.
History
The first of the benzodiazepines, chlordiazepoxide was introduced in the 1960s. Subsequently, diazepam and other benzodiazepines followed. Initially it was believed that they were much safer than barbiturates that were more popular at the time. Hence benzodiazepines grew in popularity and by the late 1990s they were the most commonly prescribed drugs in the world. They were prescribed as anxiolytics, anti-epileptics, hypnotics and in the adjunctive management of other psychiatric conditions such as depression, psychosis and mania. But by the 1980s concerns had been raised about the risk of physical dependence to benzodiazepines and withdrawal reactions upon discontinuation. This was shown in many studies (1, 2). Subsequently, the potential of benzodiazepines to induce tolerance and dependence have been unequivocally demonstrated. As a result, there are many more restrictions placed on the prescription of benzodiazepines. However, benzodiazepines are still widely prescribed and it is not unusual to come across patients who have been on them for long periods. In such patients, it is essential to explore whether they are misusing or are dependent on them, and if so to offer suitable interventions.
Pharmacological profile
Benzodiazepines share a similar chemical structure – a heterocyclic ring consisting of a fusion between the benzene and diazepam ring systems; hence the name. Most benzodiazepines also share an aryl substitute ring (Fig 1). There is very little difference between the different benzodiazepines in their mechanism of action but they vary in their potency and pharmacokinetic profiles. Benzodiazepines occupy a specific site on the Gamma Amino Butyric Acid (GABA-A) receptor, a ligand gated ion channel, and allosterically modify its affinity to GABA. Along with GABA, benzodiazepines potentiate the opening up of gated ion channels causing an influx of chlorine ions which are negatively charged. This hyperpolarizes the neuron and thereby blocks any action potential from passing through. Thus, benzodiazepines act by potentiating the inhibitory neural mechanism of GABA. But benzodiazepines act only in the presence of GABA and are not effective directly. This is the reason why they are safer than barbiturates in overdose. GABA is one of the main neural mechanisms in the brain and contributes to 40% of the synaptic transmission. There are several variants of GABA receptors and benzodiazepines act on only a few different types. Continued use results in changes to the sensitivity of these receptors and it is proposed that this results in the development of tolerance to its clinical benefit (3). The exact mechanisms involved in the development of tolerance is, however, not very clear.
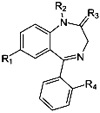
Fig 1: Structure of benzodiazepines
All benzodiazepines are absorbed orally but there is considerable variation in the half-life, bioavailability, peak plasma concentration, protein binding and metabolization products of the different benzodiazepines. The pharmacokinetic profile of the commonly prescribed benzodiazepines is detailed in Table 1. All of them cross the blood brain barrier and lipophilicity is an important marker of this function. Benzodiazepines with quicker onset of action, shorter half-life and extensive lipophilicity are more likely to be misused. When misused, benzodiazepines can be taken by mouth, inhaled as snuff or injected intravenously. Oral ingestion is the commonest route in the UK, especially in therapeutic dose dependence. Intravenous abuse is more common amongst poly-drug misusers.
Table 1. Pharmacokinetic profiles of common benzodiazepines
| Benzodiazepine | t 1/2 | Oral Bioavailability | Protein binding | Lipid solubility | Peak plasma concentration | Metabolic products |
| Lorazepam | 12 | 90% | 85-90% | Poor | 2 | No major active metabolites |
| Diazepam | 20-50 | rapidly absorbed, approximately 100% | 98-99% | High | 1/2-2 | Nordiazepam, Temazepam and Oxazepam |
| Chlordiazepoxide | 5-30 | Completely absorbed | 96% | Poor | 1-2 | |
| Temazepam | 5.3-11.5 | Readily and completed absorbed | 75-95% | 1 | No major active metabolites | |
| Nitrazepam | 24 | Well absorbed | Largely | High | 2 | No major active metabolites |
| Alprazolam | 12-15 | Readily absorbed | 80% | 1-2 | 4-hydroxyalprazolam and alpha-hydroxyalprazolam | |
| Clonazepam | 30 | 90% | 85% | 1-4 | No major active metabolites |
Definitions of misuse and dependence
Benzodiazepine misuse is included in the ICD-10 (4) under the category mental and behavioural disorders due to use of sedatives or hypnotics, and is categorised into harmful use and dependence. Harmful use is defined as continued use in a manner that produces actual harm to the physical or mental health of the person, and the harm should be directly attributable to the substance (benzodiazepine).
Dependence to benzodiazepines is defined as a cluster of behavioural, psychological and physiological symptoms and are captured in the following criteria: (Table 3).
Table 2. Criteria for dependence
| 1)Compulsion to take drugs 2)Difficulty in controlling intake 3) Evidence of physical withdrawal 4)Evidence of tolerance 5) Neglect of alternative interests 6) Continued use despite harm Presence of 3 or more of these criteria in the previous year is diagnostic of dependence |
Prevalence of benzodiazepine misuse
There are no accurate estimates of the problem and they have generally relied on data from national prescriptions and surveys of self-reported use. Most data come from the United States. The National Household Survey (5) found that about 15% of those prescribed benzodiazepines were prescribed them for long-term use (>1 year). This amounted to around 1.6% (of adults) of the general population (6). A community study conducted in the US from 1980 to 1985 found a lifetime prevalence of 1.1% for sedative, hypnotic or anxiolytic abuse or dependence (7). A Dutch study found that amongst patients prescribed benzodiazepines the lifetime prevalence for benzodiazepine dependence was 51% among GP patients and 69% amongst psychiatric outpatients (8). In the same study, the past year prevalence rates for benzodiazepine dependence using were estimated to be 40% and 63% respectively. In the UK, around 500,000 to 1 million people are prescribed benzodiazepines long term. Of these, at least 50% are estimated to be dependent on benzodiazepines (9).
Key features of benzodiazepine misuse and dependence
The most commonly misused benzodiazepines in the UK are diazepam and temazepam and the most common pattern of use in therapeutic dose dependence is oral ingestion. Kan et al (10) studied risk factors for benzodiazepine misuse and identified the following: longer duration of treatment, higher doses, use of more potent benzodiazepines, shorter acting drugs and a history of anxiety problems. Patients who have a previous history of other substance misuse or mental illness also have an increased risk of developing benzodiazepine misuse/dependence.
It is likely that for most of these patients, benzodiazepines would have been prescribed for medical reasons. The prescription would then have been continued for their perceived effectiveness or the dosage would have been increased. With the development of tolerance, therapeutic benefit may be limited but continued use may persist to relieve withdrawals. Tolerance has been noted to develop at different rates to the different clinical effects of benzodiazepines. Tolerance to hypnotic, anti-epileptic and amnesic effects are seen quickly (9). Controversy surrounds the development of tolerance to the anxiolytic effects as some studies have shown that long term use of some benzodiazepines do not result in loss of treatment efficacy (11). Some of the other pointers towards dependent use may be reliance on regular prescriptions, dosage escalation, unsuccessful attempts to cut-down or stop drug use and high anxiety levels (9). Occasionally, the patient may ‘top-up’ prescribed benzodiazepines with illicit benzodiazepines. It may sometimes be difficult to distinguish whether continued use is of therapeutic benefit or only acting to relieve withdrawals. In some patients, when attempts are made to reduce or stop these prescriptions, they may change doctors or even ‘doctor –shop.’
Assessment
It is important to individualize assessments as presentation can vary significantly. It is important to explore the reason/s why the benzodiazepine was started, duration of treatment, drug formulation, history of dose escalation and effectiveness (symptomatic) of continued benzodiazepine use: both subjective and objective. Previous attempts to stop (by self or by the prescriber) benzodiazepines and their outcomes are important pointers to the severity of the problem and may also give a clue about the nature of withdrawal reactions. Other important aspects to be covered in the assessment are: history of alcohol and other drug misuse, psychiatric illnesses such as anxiety, depression and personality disorders.
Understanding and assessing the pattern of use of benzodiazepines, its dose, duration of treatment and continued efficacy are very important. Long term use can result in physical dependence, tolerance and withdrawal reactions. But, these in themselves do not constitute misuse or dependence. Therefore, it is important to look for other symptoms of misuse/dependence for example: craving, compulsion, continued use despite harm and neglect of alternate interests (Table 3). The presence or absence of these features will significantly influence management.
It is important to assess the risk and severity of potential withdrawal symptoms. Physical withdrawal is observed after continuous use of benzodiazepines for 8 weeks or more (2). There is even some suggestion that continued use for 4 weeks would lead to dependence. The nature of withdrawal reaction varies according to the type of benzodiazepine, dosage and the duration of consumption. Use of short acting benzodiazepines, high doses and longer duration of consumption pose greater risks of withdrawal reaction. Other factors increasing the risk of withdrawal reactions are use of high potency benzodiazepines, presence of psychiatric or personality disorder (12), and chronic physical health problems such as epilepsy, chronic pain, etc. The nature of withdrawal reactions vary and can last for 5 to 28 days, peaking in severity at 2 weeks. Table 2 lists some of the symptoms associated with benzodiazepine withdrawal.
Table 3. Benzodiazepine withdrawal symptoms
Anxiety Derealisation |
Finally, consider seeking advice or referral to specialist services if there is a history of alcohol or other drug misuse, severe personality or psychiatric disorders, co-morbid physical illnesses and if there is history of withdrawal seizures. Withdrawal seizures occur rarely in therapeutic dose misusers (13).
Management
In a minority of patients, benzodiazepines continue to retain their efficacy even after prolonged use. This can especially be the case for their anxiolytic effects and so continued use may be a viable option if there are no risk factors. This decision should only be arrived at after weighing the risks and benefits of continued prescription and alternate options and it should be reviewed at regular intervals.
If the assessment suggests harmful use or dependence, it is important to raise these concerns with the patient. It is useful to explore the patient’s attitude to continued prescription and provide information regarding the harms of continued use, along with the benefits of stopping benzodiazepines. Concerns, especially about the nature of withdrawal reaction should also be promptly addressed. It is crucial to engage the patient the decision making process and in planning a future treatment regime. Patient readiness and motivation to address the misuse are essential to the success of any attempt to reduce and/or stop the benzodiazepine.
The most frequently used pharmacological intervention in the management of benzodiazepine misuse and dependence is to switch to the equivalent doses of a long acting benzodiazepine, such as diazepam (Table 4) and then to gradually reduce and stop. The standard recommendation is to reduce by one eighth every fortnight, and more gradually at lower doses (BNF). It may take up to several months to complete the withdrawal and sometimes, it may be necessary to slow the pace, especially if the patient is struggling with reductions. It is important to regularly review and monitor for withdrawal symptoms. Reassuring the patient that symptoms of withdrawal are temporary can be very helpful.
Table 4. Equivalent doses of Diazepam 5 mg
| chlordiazepoxide 15 mg loprazolam 0.5–1 mg lorazepam 500 micrograms lormetazepam 0.5–1 mg nitrazepam 5 mg oxazepam 15 mg temazepam 10 mg |
If there is established dependence, the patient will need additional support during the preparation and withdrawal stages. Interventions such as relaxation training, regular exercise and complementary therapies such as aromatherapy have been found to be beneficial. Relapse prevention work is also essential in this group of clients.
Denis et al (14) in a systematic review found good support for the gradual and progressive withdrawal. This review however did not find evidence to support switching from short-acting to a long-acting preparation. In a similar review, Parr et al (15) found that psychological interventions along with gradual dose reduction were more effective than routine care.
Finally, it is also important to consider alternative medications to treat anxiety disorders. NICE (16) recommends using antidepressants such as paroxetine and venlafaxine as first line drugs for the management of anxiety disorders.
Flumazenil in the treatment of benzodiazepine dependence
Flumazenil is a partial benzodiazepine agonist and that is used in the management of benzodiazepine toxicity. At low doses, it does not have any intrinsic agonistic activity. But it blocks other agonist and inverse agonists from acting at the receptor site. It has been shown to be useful in benzodiazepine withdrawal and dependence in three studies. Saxon et al (17) conducted a double-blind pilot study of 10 patients who were benzodiazepine dependent and found that flumazenil reduced withdrawal symptoms. Gerra et al (18) compared it with oxazepam (in tapering doses) and placebo in 20 patients with benzodiazepine dependence and found it to reduce withdrawal symptoms significantly. In a very recent study, Hood et al (109) looked at its effectiveness in an open trial of 13 benzodiazepine dependent subjects and found no differences in the nature and severity of withdrawal symptoms between subjects but significant abstinence from benzodiazepine was noted post treatment. Despite all this, flumazenil is not yet licensed for the treatment of benzodiazepine dependence.
Conclusion
Benzodiazepine misuse or dependence is common among patients who have been prescribed them for long periods. Current evidence supports gradual and progressive withdrawal of benzodiazepines and addition of psychological interventions for the management of misuse.
References
1. Tyrer P, Rutherford D, Higgit T (1981). Benzodiazepine withdrawal symptoms and propanolol: Lancet 1: 520-522
2. Petursson H, Lader MH (1984). Benzodiazepine dependence: British Journal of Addiction 76: 133-145
3. Bateson AN (2002). Basic pharmacologic mechanisms involved in benzodiazepine tolerance and withdrawal: Current Pharmaceutical Design 8: 5-21
4. World Health Organization (1993b) The ICD-10 Classification of Mental and Behavioural Disorders. Diagnostic Criteria for Research. World Health Organization, Geneva.
5. NIDA (1982). National Household Survey on Drug Abuse, 1979-1981. Rockville, Maryland: NIDA.
6. Mellinger, G. D.; Balter, M. B. & Uhlenhuth, E.T (1984). Prevalence and co-relates of the long-term regular use of anxiolytics: Journal of American Medical Association 251(3): 375-379
7. Wilford, B. B. (ed.) (1990). Balancing the response to prescription drug abuse. Report of a national symposium on medicine and drug policy. Chicago, IL, American Medical Association, Department of Substance Abuse.
8. Kan, C. C.; Breteler, M. H. M.; Zitman F. G.(1997); High prevalence of benzodiazepine dependence in out-patient users, based on the DSM-III-R and ICD-10 criteria: Acta Psychiatrica Scandinavia 96(2): 85-93
9. Ashton H (2005). The diagnosis and management of benzodiazepine dependence: Current opinion in Psychiatry 18: 249-255.
10. Kan C. C.; Hilberink S. R.; Breteler M. H.(2004); Determination of the main risk factors for benzodiazepine dependence using a multivariate and multidimensional approach: Comprehensive Psychiatry 45(2): 88-94
11. Uhlenhuth, E H.; DeWIT, H.; Balter, M B.; Johanson, C E.; Mellinger, G D (1988); Risks and Benefits of Long-Term Benzodiazepine Use: Journal of Clinical Psychopharmacology 8: 161-167
12. Murphy SM and Tyrer P (1991); A double-blind comparison of the effects of gradual withdrawal of lorazepam, diazepam and bromazepam in benzodiazepine dependence: The British Journal of Psychiatry 158: 511-516.
13. Busto U E., Sellers E M.(1991), Anxiolytics and sedative/hypnotics dependence: Addiction 86(12): 1647 -1652
14. Denis C, Fatseas M, Lavie E, Auriacombe M (2006); Pharmacological interventions for benzodiazepine mono-dependence management in outpatient settings: The Cochrane Library. Issue 3. John Wiley & Sons, Ltd.
15. Parr, J.M., Kavanagh, D.J., Cahill, L. et al. (2009) Effectiveness of current treatment approaches for benzodiazepine discontinuation: a meta-analysis. Addiction 104(1), 13-24.
16. NICE (2007). Anxiety: management of anxiety (panic disorder, with or without agoraphobia, and generalised anxiety disorder) in adults in primary, secondary and community care. CG22. London. NICE. April 2007.
17. Saxon L., Hjemdahl P, · Hiltunen A J, Borg S. (1997); Effects of flumazenil in the treatment of benzodiazepine withdrawal. a double-blind pilot study: Psychopharmacology 131 : 153.160
18. Gerra G; Zaimovic A; Giusti F; Moi G; Brewer C. (2002); Intravenous flumazenil versus oxazepam tapering in the treatment of benzodiazepine withdrawal: a randomized, placebo-controlled study: Addiction Biology 7( 4) 385 – 395.
19. Hood S, O’Neil G & Hulse G. (2009); The role of flumazenil in the treatment of benzodiazepine dependence: physiological and psychological profiles: 23(4) 401–409.
Copyright Priory Lodge Education Ltd. 2010
First Published June 2010
priory Useful links
Click
on these links to visit our Journals:
Psychiatry
On-Line
Dentistry On-Line | Vet
On-Line | Chest Medicine
On-Line
GP
On-Line | Pharmacy
On-Line | Anaesthesia
On-Line | Medicine
On-Line
Family Medical
Practice On-Line
Home • Journals • Search • Rules for Authors • Submit a Paper • Sponsor us
All pages in this site copyright ©Priory Lodge Education Ltd 1994-


