Browse through our Journals...
Secondary Sexual Dysfunction and Antipsychotics
Survey of Psychiatrists in Greater Manchester
Dr Inderpreet Singh, Dr Simon Sandhu, Bindweep Kaur
About the Authors
Dr Inderpreet Singh MBBS MCRPsych DMH
Staff Grade Psychiatrist, Pennine Care NHS Foundation Trust
Dr Simon Sandhu MB ChB MRCPsych
Consultant Rehabilitation Psychiatry, Pennine Care NHS Foundation Trust
Bindweep Kaur BHMS DHM
Public health analyst NHS North West, Manchester
Abstract
Sexual side-effects (SSEs) of antipsychotics are one of the major causes of non compliance and its assessment and management is important to improve quality of life. However, the assessment of sexual side effects continues to be neglected. A survey of all psychiatrists in 2 major mental health trusts of Greater Manchester was conducted to ascertain the awareness and attitudes of psychiatrists towards the assessment and management of sexual side effects of antipsychotics. An online survey was sent to all psychiatrists working in Pennine Care and Greater Manchester West NHS Foundation Trusts. All responses were analysed using Microsoft Excel.
Almost one quarter (24%) of junior doctors (ST/CT1-3) were unaware of any SSEs caused by antipsychotics and only 23% of the respondents thought that assessment of SSEs was very important. However, 54% of the total respondents did not regularly assess SSEs of which 40% were consultants. None of the respondents used a validated scale to assess SSEs. Thirty four percent of the respondents were not aware of the medications that can be used to manage SSEs of whom 59% were ST1-3. Prominent barriers to assessing SSEs included lack of training and limited understanding of symptoms.
There is a clear lack of awareness amongst core trainees regarding SSEs which needs to be addressed through MRCPsych curriculum and clinical supervision. To improve compliance and the quality of life of these vulnerable patients, a concerted approach of increased recognition, proactive assessment, specific training, MDT input and evidence based practice is required.
Declaration of interest
None
Introduction
Sexual side-effects (SSEs) of antipsychotics are one of the common and major causes of sexual dysfunction in patients with schizophrenia with a significant negative impact on their quality of life (Olfson M et al, 2005) and compliance with medication (Montejo AL et al, 2001, Fleischhacker WW et al, 1994, Perkins DO, 2002, Lambert M et al, 2004). The estimated prevalence of SSEs ranges from 25% to 60% depending upon the antipsychotic agent (Demyttenaere K et al, 1998) and is believed to affect both genders more or less equally (Hong L et al, 2009). The occurrence of SSEs and their effect on patients' quality of life has long been known, however, they have not been well studied and their assessment and management is still neglected (Malik, P, 2007, Segraves RT, 1989, Smith SM et al, 2002). Moreover, the prevalence of sexual dysfunction in patients treated with antipsychotics has been under-reported, primarily due to the hesitancy of patients and psychiatrists to discuss this issue (Hellewell JSE, 1998, Peuskens J et al, 1998).
Although both typical and atypical antipsychotics have been implicated for SSEs, there is a noticeable difference in prevalence of SSEs between conventional and atypical antipsychotics, as well as identifiable differences amongst the atypical group primarily due to their mechanism of action on Dopamine pathways (Martin D et al, 2006). Postulated mechanisms of development of SSEs due to antipsychotics range from varied individual susceptibility, decreased dopaminergic transmission and increased prolactin levels to anticholinergic effects and action on peripheral receptors causing problems with erection and ejaculation and reduced sexual desire due to antipsychotic-induced sedation and weight gain (Taylor D et al, 2007).
There are various factors hypothesised in the literature for reductions or omissions in the assessment of SSEs ranging from misconceptions that people with schizophrenia are unable to manage their sexuality (Akhtar S et al, 1977, Erlenmeyer-Kimling L et al, 1969) to more plausible and evidence based explanations such as a lack of awareness in staff, reluctance by staff and patients to discuss this concern and the impact of cultural and religious factors (Bhugra D et al, 1993). Clinicians may find it difficult to enquire about this problem and patients often hesitate to complain (Clayton AH, 2001). Moreover, when detected, there is often a decreased emphasis on its management and sometimes a lack of adequate specialist services or a clear pathway.
Understandably, in an otherwise well and stable patient, there is an increased emphasis to adopt a cautious approach towards the management of SSE by not switching antipsychotics or reducing dose, which unfortunately compounds the problem. Recent studies have confirmed previously reported observations that psychiatrists frequently underestimate sexual dysfunction and a discrepancy between the patient and psychiatrist’s perception of sexual dysfunction was noted (Martin D et al, 2006). Other factors including a lack of confidence and training amongst professionals could also be implicated as a contributing factor to the ongoing cautious or ‘wait and watch’ approach (Romanus NN et al, 2008).
Method
A mixed method cross sectional online survey with quantitative and qualitative elements was disseminated to all psychiatrists, including Consultants, Staff and Associate Specialist (SAS) doctors and trainees working in Pennine Care and Greater Manchester West NHS Foundation Trusts, to reduce the sampling error and increase the reliability of the study. The project was approved and registered by the individual Trust’s Research and Audit panels. A list of all eligible participants was populated using medical HR records and the survey was distributed through the clinical audit and HR department of the respective trusts. A 15-item online questionnaire was designed using the ‘Survey Monkey’ website and all participants were contacted via email with a link to complete the survey online. Efforts were made to ensure that the questionnaire was unambiguous, well structured and well worded, to increase the validity of the study. All responses were collected anonymously to maintain confidentiality and reduce bias. Further reminders were sent during the survey to improve the participation.
Questionnaire
The data collection tool aimed to obtain information from participants regarding their gender, years of psychiatric experience, grade, awareness of any sexual side effects of antipsychotics, frequency of assessments of SSEs, the rationale of the assessment and use of any screening tools. In addition, there were questions relating to non compliance due to SSEs, barriers in assessing SSEs as well as the management approach employed by clinicians.
Analysis
Data analysis was performed using Microsoft Excel to compare and contrast practice among clinicians based on 4 grades: Consultants, SPR or ST4-6, Staff Grade and Associate Specialist doctors, and SHO or ST/CT 1-3. Confidence intervals were calculated using the Wilson Score method, which has been evaluated and recommended by Newcombe and Altman, (Newcombe RG et al, 2000) to increase the validity of the study (Association of Public Health Observatories, 2008).
Results
Participants
Overall response rate was 42.2% (n=65) of which 55% were male and 45% female.
Awareness
Almost one quarter (24%) of junior doctors (ST/CT1-3) were unaware of any SSEs caused by antipsychotics, although all the senior psychiatrists (Consultants, SAS and ST4-6) were aware.
Surprisingly, about half (49%) of the respondents were not aware of the 4 phases of normal human sexual response of which 53% were consultants. Fifty four percent of respondents reported SSEs to be more common in males whereas 45% (n=29) reported both genders being affected. Just over half of the participants (54%) felt that SSEs were associated with both typical and atypical antipsychotics, however, only 29% (n=5/17) of the ST1-3 and 56% (n=5/9) of ST4-6 were aware of this.
Assessment
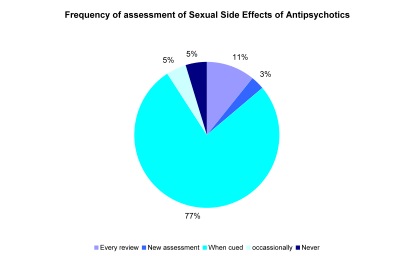
Eighty two percent of ST1-3 and 54% (of which 40% were consultants) of the total respondents did not regularly assess patients for SSEs with only 23% (n=15/35) of the participants considering assessment of SSEs to be very important during psychiatric assessment. The majority (77%) of the respondents assessed their patients for SSEs only ‘if suspected’ or complained of by the patient and none of the psychiatrists employed a validated scale like The Arizona Sexual Experiences Scale (ASEX) or the Liverpool University Neuroleptic Side Effect Rating Scale (LUNSERS).
About one-fifth of the participants reported that they never monitored prolactin levels of which 54% were consultants. The rest had varying views regarding monitoring prolactin levels ranging from every 3 months to yearly to ‘when indicated’. According to Maudsley guidelines, depending on the anti-psychotic prescribed, prolactin should be monitored at baseline, then every 6 months and yearly thereafter. However, prolactin-sparing anti-psychotics such as Aripiprazole, Clozapine and Olanzapine do not require mandatory monitoring.
Management
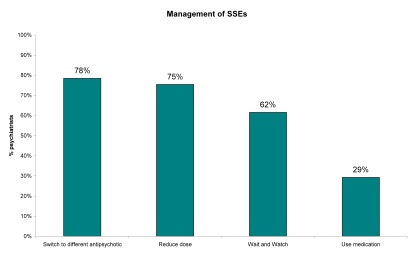
The majority of the respondents (78%) managed the SSEs by switching to a different anti-psychotic followed very closely by reducing the dose of the antipsychotic (75%) and employing the ‘wait and watch’ regime (62%). Only 29% used medication to manage sexual dysfunction, however, about a third (34%) of the total respondents were not aware of the medications that can be used to manage SSEs of whom 59% were ST 1-3.
In addition, most of the respondents (78%) reported experiencing poor compliance due to SSEs.
Barriers
Of the list of barriers to assessment outlined in the questionnaire, the majority of respondents (85%) highlighted hesitancy or unwillingness of the patients to disclose information as the main barriers in assessing SSE. However, lack of knowledge and a need for more training were also outlined as other major barriers as almost half (49%) of the respondents reported having limited understanding of the symptoms or diagnosis of SSEs.
The participants were given an option to comment on other barriers they face in assessing SSEs in their day-to-day practice and we have classified them under 2 headings: Related to and not related to training. Surprisingly, most of these barriers were training related and were mostly identified by consultants as outlined below.
Barriers to assessing SSEs (options provided in the questionnaire)
Unwillingness to disclose by the patients 85%
Limited understanding of the symptoms/diagnoses 49%
Hesitation of the clinician 63%
Fear of offending 37%
Time constraints 45%
Opposite sex doctors 42%
Other barriers outlined by participants-
Related to training
1. Not viewed as a priority by some clinicians
2. Lack of knowledge of clinicians, embarrassment, not seeing them as important
3. Not recognised by clinicians
4. No training
5. Very hard to do in patients with poor English or via a translator
6. Accessing sexual disorders clinic, limited guidance on management
7. Impression that not a problem on low doses e.g. quetiapine 50mg
8. In under 16s disclosure of sexual activity may raise safeguarding issues
Not related to training
1. Hypo-sexuality is not seen as an issue by the family/carer of my patient group (Learning Disability)
2. Unwillingness to change antipsychotic the patient is stable on
3. Patient/doctor age differences, cultural issues, number of people in room e.g. partner/CPN etc
4. Related to unwillingness to disclose - adolescents might not want their parents to know that they are sexually active.
Additional comments made by participants revealed that the respondents are aware that sexual side effects are underreported and under-treated and can lead to non-compliance and therefore more needs to be done. However, they are concerned that they don’t have the appropriate training on various issues on how to deal with it and on appropriate management plans. Concerns were also raised on the time needed to assess each patient. However, it has been recognised that more training on SSEs would lead to a better quality of care for the patients.
Some of the interesting comments were:
1. If the patients have sexual side effects, but the symptoms are well controlled with the current medication, you know that the medication is the offending agent, what will you do, do you change medication?
2. It is a dilemma. Furthermore, the cost of treatment for sexual side effects, the PCT may not be keen to fund such treatments.
3. I would like information / training on the appropriateness / success of using Cialis etc for sexual dysfunction with antipsychotic medicines.
4. There should be guidelines on how to ask or monitor for sexual side effects in ethnic populations where it may adversely affect the Dr -pt relationship i.e. female white junior Dr asking Muslim male patient about erections.
5. I believe this may be a significant issue related to non-compliance.
6. We need to address this issue as I believe that it can seriously impact on compliance and the development of sexual dysfunction may aggravate any symptoms e.g. depression, paranoia.
7. Often underplayed and ill recognised. Have discussed with colleagues who attribute a lesser importance, but I find lots of patients suffer, although more likely to keep taking if informed before and concerns taken seriously.
8. This is an important area of inquiry. However, any mandatory increases in information gathering can only lead to have more time with each patient than the paltry 20 minutes with each patient. This has to be recognised - as sexual side effects are one of many unwanted effects and we need to be monitoring for all of them. This will all take time but will improve the quality of our care.
9. Dose reduction, drug holidays, adjunctive medication, switching to another drug should be tried but the Cochrane Reviews suggest Sildenafil on limited evidence so that is what I use even though it makes Mr xyz uncomfortable.
10. Training and awareness needed
11. Risperidone is particularly bad in young men
12. Work with older people exclusively and often with dementia so this area is often not so relevant. In those without dementia I do think we should consider it more although our pt group are less likely to discuss this issue.
13. An important area of non-compliance under-reported and under-treated
14. It is really difficult to discuss with teenagers, particularly when cultural sensitivity is also needed
Limitations of the study
The study had a modest response rate of 42% which is not uncommon in online surveys (Colleen C et al, 2000). Although this study was done in 2 major mental health trusts in Greater Manchester, it cannot be said that results are generalisable. The study included all the psychiatrists working in different sub-specialities of psychiatry which may reflect differences in experience, awareness and management of SSEs among senior clinicians, for example, clinicians working in learning disabilities, old age or child and adolescent psychiatry may be less exposed to experience or manage SSEs. Nevertheless, awareness regarding SSEs is important for every psychiatrist, not only for clinical but also for academic reasons as senior clinicians often supervise junior doctors who may need support in this area.
It can not be asserted that this was an all-inclusive survey and the data collection tool was comprehensive enough to record all the important and relevant information. Although realistic effort was made to ensure normal and routine clinical practice be recorded rather than ‘what should be done’ i.e. academic information from national guidelines, the impact of social desirability bias should be taken into account. In addition it cannot be inferred that the responses reflect actual clinical practice as they were based on completed self-reported questionnaires.
Discussion
This study specifically focuses on sexual side effects attributed to antipsychotics which are an important and potentially reversible cause of sexual dysfunction in patients with schizophrenia.
This study makes some interesting observations:
First, there is a significant gap in the knowledge base regarding the occurrence of SSEs particularly amongst junior doctors as well as inconsistent awareness regarding their incidence due to atypical agents. For example, only about half of the total psychiatrists surveyed reported that SSEs are associated with both typical and atypical agents and similar proportion felt that both genders are affected. This is an important finding as having proper awareness of this issue is crucial to any future assessment carried out by clinicians, more so for junior doctors as they are often the first point of contact for patients experiencing these distressing side effects.
Second, there is far less emphasis given to regular assessment of SSEs which further substantiates similar findings in pervious studies (Romanus NN et al, 2008). More than half of the total respondents did not regularly assess their patients for SSEs and only about a quarter considered SSEs assessment to be a very important aspect of psychiatric assessment. The considerable variation in the reported frequency of prolactin monitoring is also a cause of concern as about one fifth (17%) of the participants reported that they never monitored prolactin levels of which 54% were consultants. This was despite the majority of respondents reporting poor compliance due to SSEs.
Third, there is increased recognition that specific training and skills are required to improve assessment and management of SSEs as identified by the respondents. Lack of knowledge was not only highlighted as one of the important barriers but almost half of the clinicians reported having limited understanding of symptoms to diagnose SSEs.
Finally, this survey reconfirms the long standing view that assessment and management of SSEs is still neglected. Although increased experience is directly related to increased awareness in clinicians, there is still a need to re-emphasise that the management of SSEs is very important and should be part of every psychiatric assessment. Previous studies have also highlighted the need for training and increased recognition of SSEs in main stream psychiatry (Romanus NN et al, 2008).
Conclusions
This study contributes to the existing pool of evidence that SSEs needs to be given equal, if not more importance than other common side effects of antipsychotics. There is a need to include it in every psychiatric assessment and training needs to be provided to trainees and other doctors to assess and manage SSEs without the fear of offending others or feeling embarrassed. Perhaps it could be introduced conspicuously in the MRCPsych curriculum as an Objective Structured Clinical Examination station or as a distinct Work Place Based Assessment. Furthermore, the barriers identified need to be carefully addressed and popular teaching aids such as e-modules could be developed to re-emphasise clinicians of their importance. Other options suggested in previous studies including developing a training package and regular use of validated questionnaires will also aid improved detection. Where appropriate a multidisciplinary approach can also be employed to help ensure improved detection and to address barriers such as cultural and sensitivity issues, opposite gender doctors and hesitancy on the part of patients; the propensity of patients to confide in the ‘named nurse’ should be carefully utilised.
Therefore a concerted approach of increased recognition, proactive assessment, specific training, MDT input and evidence based practice will greatly improve the quality of life for these vulnerable patients. Perhaps there is a need for a ‘paradigm shift’ in recognising the sexual needs of patients with serious mental illness and thence the need to proactively work towards improving their quality of life (Eric RW et al, 2007).
References
1. Akhtar S, Crocker E, Dickey N et al. (1977) Overt sexual behaviours among psychiatric inpatients. Diseases of the Nervous System. 38, 359-361
2. Association of Public Health Observatories. (2008) Technical briefing 3: Commonly used public heath statistics and their confidence intervals. HMSO
3. Bhugra D. & De Silva P. (1993) Sexual dysfunction across cultures. International Review of Psychiatry. 5, 243–252.
4. Clayton AH. (2001) Recognition and assessment of sexual dysfunction associated with depression. Journal of Clinical Psychiatry. 62 (Suppl. 3), 5-9.
5. Colleen C, Fred H and Russel L. Thompson. (2000) A Meta-Analysis of Response Rates in Web- or Internet-Based Surveys. Educational and Psychological Measurement. 60, 821
6. Demyttenaere K, De Fruyt J, & Sienaert P. (1998) Psychotropics and sexuality. International Clinical Psychopharmacology. 13 (Suppl. 6), 35–41.
7. Eric RW, Dustin EW, Brea LP, Carrie EF. (2007) Stigma and the Sexual Isolation of People with Serious Mental Illness. Social Problems. 54(1), 78–98.
8. Erlenmeyer-Kimling L, Nicol S, Rainer JD et al. (1969) Changes in fertility rates of schizophrenic patients in New York State. American Journal of Psychiatry. 125, 916-927.
9. Fleischhacker WW, Meise U, Gunther V, Kurz M. (1994) Compliance with antipsychotic drug treatment: influence of side effects. Acta Psychiatr Scand. 382, 11–15.
10. Hellewell JSE. (1998) Antipsychotic tolerability: the attitudes and perceptions of medical professionals, patients and caregivers towards side effects of antipsychotic therapy. Eur Neuropschopharmacol. 8, 248
11. Hong L, Bruce JK, Christopher JT, Jennifer S and Jan V. (2009) Sexual dysfunction in patients with schizophrenia treated with conventional antipsychotics or Risperidone. Neuropsychiatr Dis Treat. 5, 47-54
12. Lambert M, Conus P, Eide P, et al. (2004) Impact of present and past antipsychotic side effects on attitude toward typical antipsychotic treatment and adherence. Eur Psychiatry.19, 415–422
13. Malik, P. (2007) Sexual dysfunction in schizophrenia. Current Opinions in
Psychiatry. 20, 138-142.
14. Martin D, Yulia D, Sebnem P, Martin A, Afaf K, Aleksander A et al. (2006) Effects of atypical and typical antipsychotic treatments on sexual function in patients with schizophrenia: 12-month results from the Intercontinental Schizophrenia Outpatient Health Outcomes (IC-SOHO) study. European Psychiatry. 21(4), 251-258
15. Montejo AL et al. (2001) Incidence of sexual dysfunction associated with antidepressant agents: a prospective multi-centre study of 1022 outpatients. J Clin Psychiatry. 62(Suppl 3), 10–21.
16. Newcombe RG, Altman DG (2000). Proportions and their differences. In Altman DG et al. (eds). Statistics with confidence (2nd edn). London: BMJ Books. 46-8
17. Olfson M, Uttaro T, Carson WH, Tafesse E. (2005) Male sexual dysfunction and quality of life in schizophrenia. J Clin Psychiatry. 66(3), 331-8
18. Perkins DO. (2002) Predictors of noncompliance in patients with schizophrenia. J Clin Psychiatry. 63, 1121–8
19. Peuskens J, Sienaert P, De Hert M. (1998) Sexual dysfunction: the unspoken side effect of antipsychotics. Eur Psychiatry. 13 (Suppl 1), 23–30
20. Romanus NN and Trevor F. (2008) Sexual dysfunction and schizophrenia: psychiatrists’ attitudes and training needs. Psychiatric Bulletin. 32, 208-210
21. Segraves RT. (1989) Effects of psychotropic drugs on human erection and ejaculation. Arch Gen Psychiatry. 46, 275–84
22. Smith SM et al. (2002) Sexual dysfunction in patients taking conventional antipsychotic medication. Br J Psychiatry. 181, 49–55.
23. Taylor D, Paton C, Kerwin R. (2007) Maudsley prescribing guidelines 9th edition. Taylor and Francis
First Published May 2010
Copyright Priory Lodge Education Limited 2010 -
Click
on these links to visit our Journals:
Psychiatry
On-Line
Dentistry On-Line | Vet
On-Line | Chest Medicine
On-Line
GP
On-Line | Pharmacy
On-Line | Anaesthesia
On-Line | Medicine
On-Line
Family Medical
Practice On-Line
Home • Journals • Search • Rules for Authors • Submit a Paper • Sponsor us
All pages in this site copyright ©Priory Lodge Education Ltd 1994-


