Browse through our Journals...

Schizophreniaby Dr B Green, Hon. Senior Lecturer, University of Liverpool, UK IntroductionSchizophrenia is often a chronic relapsing psychotic disorder that primarily affects thought and behaviour. It can be well-controlled with antipsychotic drugs, (sometimes called neuroleptics). The general practitioner may be called in to assess new cases of schizophrenia (incidence of 18/10,000 per year), or to provide care for the homeless mentally ill (Timms & Fry, 1989) or to provide long-term cover for rehabilitation or long-stay hostels and for families with members who have schizophrenia. Long-term community care is delicately balanced between primary care, community psychiatrists and social services. |
|
| Treatment Resistant Schizophrenia | |
Benzodiazepines
in Schizophrenia Thirumalai & Martin |
|
Learning Points
- Schizophrenia mainly affects thought and behaviour, as opposed to affect. It is often a chronic disorder in that there are multiple acute episodes and between these residual effects.
- The diagnosis of schizophrenia is usually made with the help of a longitudinal view of the patient i.e. the form of the illness is as important as the content of the illness in making a diagnosis.
- Schizophrenia affects up to 1% of the population (up to 600,000 people in the UK). Given that it is often a chronically disabling condition it is therefore responsible for a great deal of the population's morbidity. It has an incidence of 18 - 20 cases per 100,000 per year. Its peak age of onset differs for men and women. The average age of onset for men is 20-25 and the average age of onset for women is 25-20. In social terms chronic illnesses generally consume much of the total health budget. The cost of psychiatric health care has trebled in the last 20 years. In the United States schizophrenia consumes 35-40 billion dollars per year in direct and indirect costs. In the UK, direct and indirect annual costs total œ3.5 million.
Clinical Features
Concepts of what schizophrenia actually is change with time. Different names and different criteria have been used to make the diagnosis at different times. This may be because the disease itself changes with time, or because we are actually analysing a phenomenon with several different causes that all present a common picture i.e. of disturbances of thought and behaviour. Prior to this century patients with General Paralysis of the Insane (GPI) caused by Treponema pallidum were classed in with schizophrenic-like patients. It may be that what we term schizophrenia today is a heterogenous disease with different causes.
The Concept of Schizophrenia
An illness like schizophrenia has been variously described over the years. Falvet in 1851 called it Folie circulaire, Hecker in 1871 called it Hebephrenia, Kahlbaum in 1874 described Catatonia (a movement disorder) and Paranoia. Kraepelin in 1878 pulled the various concepts together into one disease entity which he termed Dementia praecox and said there were four types : simple, paranoid, hebephrenic and catatonic, depending on the clinical presentation. Simple dementia praecox involved a slow social decline, with apathy and withdrawal rather than florid psychotic symptoms - such people became drifters or tramps. Paranoid dementia praecox involved fear and systematised persecutory delusions. The Hebephrenic type was silly and facetious. (Such terms enter common usage, with their meaning slightly shifted - hebephrenia was misappropriated by the public an corrupted to the phrase 'heebie-jeebies') Catatonic patients were those with predominant motor symptoms - increased muscle tone, preservation of posture (patients could be manipulated like passive mannequins into unusual postures which they would maintain for hours), waxy flexibility, and fear. Despite their persistent immobility such catatonic patients were acutely aware of their surroundings. Before suitable pharmacological treatments arrived, unless the catatonic episode aborted spontaneously the patient would die through starvation, or thirst unless carefully nursed.
Bleuler, in 1908, criticised the use of the term dementia praecox, because he said that there was no global dementing process. He first used the term schizophrenia and said that there were four characteristics:
- blunted Affect
- loosening of Associations
- Ambivalence
- Autism
These characteristics were called the 'fours A's'. Blunted affect referred to a restricted range of affect. Loosening of associations referred to the thought disorder present in schizophrenia. Ambivalence, or an inability to make decisions was often seen in untreated cases were patients might hover for hours on the threshold of a doorway, uncertain whether to come in or go out (sometimes called ambitendence). Autism referred, not to the childhood condition, but to a retreat into an inner world, incomprehensible to the outsider.
The four diagnostic criteria of Bleuler have been revised over the years. Kurt Schneider listed the so-called 'first rank features' of schizophrenia in 1959. One of these, in the absence of organic disease, persistent affective disorder, or drug intoxication, was sufficient for a diagnosis of schizophrenia.
- third person auditory hallucinations (running commentaries on the patient's actions or thoughts, or arguments about the patient)
- thought echo [echo de la pensee], thoughts spoken out loud [gedankenlautwerden]
- passivity phenomena (made actions, made emotions, made impulses)
- thought insertion, withdrawal, broadcasting
- delusional perception
However, the criteria were criticised for being too narrow and only looking at a 'snapshot' of a patient at one point in time.
The current guidelines used are those of ICD-10 from 1992:
"A minimum requirement is one of the following symptoms: thought echo, insertion, withdrawal, broadcasting, passivity phenomena, delusional perception, third person hallucinations, and persistent delusions - all in clear consciousness.
Other symptoms used to make the diagnosis (2 must be present) include persistent hallucinations in any modality, thought blocking, thought disorder, catatonic behaviour, negative symptoms, loss of social function."
Symptoms should have been present for at least one month. This emphasis on the form of the illness helps exclude patients with transient psychotic symptoms or signs. Affective disorder should have been excluded. Symptoms should be present in the absence of overt brain disease, drug use, or epilepsy ( which can all mimic schizophrenia). ICD-10 lists the following types paranoid, hebephrenic, catatonic, residual (a chronic state) and simple.
Diagnosing Schizophrenia
Using mental state features alone (such as third person auditory hallucinations) is not a reliable way to diagnose schizophrenia. After all, psychotic features such as hallucinations and delusions can occur in affective disorders, dementia and acute organic psychoses. It is therefore important to look at the form of the illness as well as the content.
Rating Schizophrenia
Scales such as the Brief Psychiatric Rating Scale can be used to estimate the course of illness or the clinical response to treatment.
The Course of the Illness
The onset in men is earlier than in women. (20-25 c.f. 25-30). Before the illness can be recognised there is often a prodromal phase in late teenage with social isolation, interest in fringe cults, social withdrawal (e.g. living alone in their bedroom with minimal contact with family, and no friends). Patients with schizophrenia often have 'neurological soft-signs' -dysgraphaesthesia, clumsiness, movement disorders and the like. Recent research has indicated that such soft signs, dyskinesias and gait disturbances may be detectable in childhood, before the onset of florid psychotic symptoms. (Such work has investigated home movies of American children who later developed schizophrenia, and compared these with home movies of children who have not developed the disease in later life. The movies were rated by neurologists 'blind' to the subsequent diagnosis). The presence of such a 'soft-sign' in childhood is not pathognomonic of schizophrenia, but such signs are seen significantly more often in children at risk for schizophrenia. So, symptoms and signs may pre-date (by many years) the next phase, which is the 'active' phase of the illness, characterised by positive symptoms such as hallucinations, delusions, thought insertion and the like. The active phase coincides with the 'obvious' onset of the illness.
The active phase may last forever if untreated or may resolve spontaneously without treatment (although this would be very rare). Most active phases can be aborted by antipsychotic medication. After an active episode of schizophrenia there may be a complete return to normal function and no further episode may happen. It is more likely that there will be several episode through life, and that function and personality may be damaged. This impairment of function/personality may be progressive. Often the active phase with its positive features are replaced by a residual phase characterised by 'negative' features such as blunted affect or poverty of thought.
What happens to people in the years after a first episode of schizophrenia? About 20% of patients have only one episode and had no impairment of function or personality. Thirty-five per cent go on to have several episodes with no impairment between. About 10% have multiple episodes of schizophrenia with a static level of functional and personality impairment between. 35% have multiple episodes with increasing levels of impairment.
In a study which looked at the 35 year outcome of schizophrenia. 20% of those with a first episode in the 1940s were well, 45% were incapacitated by their illness. 67% had never married and 58% had never worked since their first episode.
A sixth of people with schizophrenia die by their own hand, often in response to psychotic symptoms e.g. second person auditory hallucinations telling them to kill themselves.
Features which predispose to a bad prognosis in schizophrenia
include:
- insidious onset
- neurological soft signs
- past psychiatric history
- history of violence
- long duration of first illness
- emotional blunting
- social withdrawal
- poor psychosexual functioning
In summary, a minority of a fifth of patients with a first episode of schizophrenia have a good prognosis. The majority have multiple episodes, and about half have chronic impairment of function affecting their ability to form relationships and work. Schizophrenia can therefore be seen as an chronically disabling disorder with important family and social consequences.
Aetiology
Kraepelin delineated 'functional psychoses' from 'organic psychoses'. Organic psychoses included dementias and epilepsy. Kraepelin was well aware of the pathology of the brain in such illnesses. The brain however looked normal in post-mortems of affective and schizophrenia sufferers. Hence Kraepelin called affective disorder and schizophrenia 'functional psychoses', implying there was no gross pathology to be seen in the brain. Modern neuroimaging though has found an organic basis for some affective and schizophrenic disorders (see below) and so the term 'functional psychosis' is no longer used.
For a long time, when schizophrenia was seen as a 'functional' disorder, there were doctors who advocated that the whole concept of schizophrenia was untrustworthy, and not an illness, but a sociological phenomenon - i.e. that patients with schizophrenia were normal people driven insane by an insane world. Some pointed to the role of the mother and said that some mothers' rearing behaviours were 'schizophrenogenic', i.e. that the mother's brought up their children incorrectly and induced schizophrenic thought patterns in them. They did this by using a 'double bind' eg asking the child to do something, but giving a contrary non-verbal message. Other doctors and psychologists suggested that mental illness was a 'myth'.
The efficacy of antipsychotic drugs, and recent advances in biological research have countered this 1970s concept, but difficulties with the concept of schizophrenia remain. It is possible that the people who have schizophrenia are a heterogenous group with different areas of their brains affected to varying degrees by neurochemical imbalances, neurodevelopmental problems, genetic defects, viral infections, or perinatal damage amongst other causes. Continuing research is essential. A treatable cause for a percentage of patients is worth hunting for. Prior to this century, between 10 and 30% of schizophrenia-like patients probably had neurosyphilis. Without the knowledge of neurosyphilis that we now have, this group of treatable patients would merely be a sub group of an even larger population of undifferentiated schizophrenia.
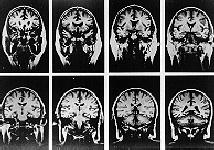
MRI Scans of a Control Subject.
Taken from Problem-Based Psychiatry
Scan by Professor Nancy Andreasen
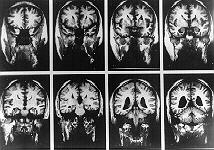
MRI Scans of a male patient with schizophrenia.
Taken from Problem-Based Psychiatry
Scan by Professor Nancy Andreasen
Recent Research Findings about the Aetiology of Schizophrenia
Severe unremitting DSM-IV schizophrenia appears to be more common in males. Females tend to have an remitting illness characterised by more affective symptomatology with later onset. Females have a better prognosis - it is not known why - hypotheses include possible antidopaminmergic actions of oestrogen - or that the aetiology of schizophrenia in males and females is different.
CT scans which larger Sylvian fissure volume can predict negative symptoms and the likelihood of unemployment, mediated by cognitive impairment.
A recent study into the British 1946 birth cohort (Jones et al, 1994) found that various factors in a cohort of 5362 children born between March 3-9 1946 were associated with later schizophrenia in 30 cases of schizophrenia occurring between 16 and 43years:
- delayed psychomotor milestones e.g. late walkers
- speech problems
- educational test scores worse on verbal and non-verbal tests at 8, 11, and 15 years.
- preferring to play alone at age 4 and 6
- rating themselves as less socially confident
- teachers rating them as more anxious
Families and Schizophrenia
Genetic Aspects If one family member has schizophrenia, the closer you are to that individual in genetic terms, the more likely you are to get schizophrenia too. In twin studies if one twin of a dizygotic pair gets schizophrenia (the case is called 'the proband'), the other twin has a 14% chance of also getting schizophrenia in his or her lifetime (lifetime risk). In a monozygotic pair the twin of the proband has a 50% lifetime risk. This shows that the higher the proportion of genetic material in common with the greater the chance of developing schizophrenia.
Spectrum Disorder
Relatives of patients with schizophrenia have been noted to have mild features of the illness themselves to a certain degree. So that relatives may have some mild loosening of associations in their everyday speech, but not to such a degree that it could be described as thought disorder. This has resulted in the idea that schizophrenia may be one extreme of a spectrum of schizophrenia-related disorders, which include language disturbance and personality differences - such as schizoid or eccentric behaviour.
The Family Environment
The emphasis on community care has meant that instead of sufferers being removed to large asylums for most of their lives, they can be accommodated in the community, within a family setting. There are advantages and disadvantages for the sufferer and the family. Some research has indicated that certain types of family environment may be harmful to the patient, but that with help characteristics of this environment can be altered to help the individual remain within the family. The environment which promoted a greater frequency of relapses is called a high expressed emotion environment. High EE environments involve a lot of negative criticism towards the patient, overinvolvement by certain members of the family, expressed hostility, and greater than 35 hours per week face-to-face contact. Education programmes for the family seek to explain features of the illness to the family, reduce the amount of hostile criticism, and 'ration' contact. Such programs have been shown to reduce EE and reduce relapse rates.
Organic evidence for Schizophrenia
Current opinion tends to favour a scenario where an early perinatal brain insult leads to dormant CNS damage which particularly manifests in the developing brain at or after adolescence (Murray et al, 1992). The perinatal damage has been linked to birth trauma and intra-uterine viral damage.
Treatment
Oral treatment with the first generation of antipsychotics (chlorpromazine, haloperidol) has been supplanted by a variety of intramuscular depot preparations. Depot injections enhance compliance, because doses can be given every few weeks by community nurses or practice personnel. Increased compliance and reduced relapse rates are useful factors for depot injections in chronic schizophrenia. Newly and recently diagnosed cases are often stabilised on oral antipsychotics before commencing on depot medication. Commonly used depot preparations include Depixol (flupenthizol) and Modecate (fluphenazine). Depixol is the most commonly prescribed depot in the UK.
Emergency behavioural control of schizophrenia can be achieved by intramuscular injections of chlorpromazine (e.g. 75- 100 mg) or haloperidol (10-20mg), but these are best given in hospital, or where admission is imminent. In many areas i.m. Clopixol-Acuphase (zuclopenthizol in a single dose of 50-150 mg) is used to gain rapid reduction in symptoms in the emergency setting.
Side-effects of conventional antipsychotics depend on the neurotransmitter systems effected. Adrenergic side-effects include postural hypotension and akathisia (an uncomfortable inner restlessness which can be modified by beta-blockers). Histaminergic side-effects include sedation. Dopaminergic side- effects include galactorrhoea, acute dystonias and Parkinsonism (abated by drugs such as oral or i.m. procyclidine). Cholinergic side-effects include dry mouth, blurred vision, hallucinations and ejaculatory dysfunction. Other side-effects include weight gain, jaundice, bone-marrow suppression, tardive dyskinesia, and the neuroleptic malignant syndrome.
The potency of conventional antipsychotics is related to their ability to block dopamine-2 (D2) receptors. However, there are a substantial minority (about 20%) of patients with schizophrenia who do not respond to these conventional neuroleptics. Clozapine, an oral drug, has been increasingly used for resistant schizophrenia in the UK since the early 1990s (although available for many years in Scandinavia). In at least a third, and possibly two-thirds of resistant cases clozapine can reduce symptoms. In this respect clozapine is something of a breakthrough. Family doctors are unlikely to come across its use for some time, since it is mainly used within secure hospitals and hospital settings. However its novel properties are worth consideration. It seems to work because of its activity at D4 and at 5-HT2 receptors rather than the conventional drugs activity at D2 receptors. The drugs has an unpleasant side-effect profile, causing neutropenia in 3.6% and agranulocytosis in 0.75%, (Atkin & Veys, 1994). A monitoring service is in place for all patients (who take the drug on a named basis). The monitoring service exists to pick up blood cell dyscrasias in the early stages whilst the bone marrow has the ability to regenerate if the drug is stopped.
Treatment is not confined to antipsychotic agents. Drugs commonly control positive symptoms better than negative ones. Negative symptoms seem to be worse in an understimulating environment. Unfortunately many bedsits and park benches are even less stimulating than the notoriously understimulating asylum back wards. However, for a substantial proportion of patients stimulating rehabilitating environments are available, sometimes via health and social services and sometimes via the voluntary or church sectors. Psychiatrists perhaps place too much emphasis on the physical management of the illness. Their patients and families place often rely more on respite care, social support, financial support, good quality housing and day care. However, overstimulating environments seem to be as bad as understimulating ones, and just like adverse life events, may provoke relapse.
The Role of the Community Psychiatric Nurse in Treatment
Some studies have cast doubt upon whether CPNs are best deployed treating non-psychotic illness. In one study GPs were equally effective as CPNs in managing neurotic disorders and did not even save time by referring patients to CPNs (Gournay & Brooking, 1994). This led the authors to suggest that CPNs should refocus their activities towards people with serious mental illness and urged them to use interventions of proven effectiveness. This begs the question: what can CPNs do for psychotic illness beyond administering depots once in a while and monitoring for relapse?
CPNs can make effective specific psychosocial interventions with patients and their families such as:
- engaging the family and patient
- organising household meetings
- family education
- improving family communication skills
- family problem solving
- dealing with drug compliance
- crisis management
- social skills training
- cognitive-behavioural strategies for depression, anxiety and other symptoms
If trained to use these skills CPNs can improve outcome through:
- improving patient symptom scores
- improving patient's social functioning
- possibly reducing inpatient episodes
- reducing minor psychiatric morbidity in carers
- improving carers' knowledge about neuroleptic medication.
(Brooker et al, 1992, 1994) Services for Schizophrenia
Entry to services Initial diagnosis is by the psychiatrist who may become involved when the patient presents to casualty for the first time, or via outpatient referral from the GP, or via domiciliary consultation requests form the GP for an assessment in the patient's home, or via calls to police stations to assess people in the police cells. Diagnosis must rule out treatable organic causes e.g. temporal lobe epilepsy, and other organic causes (e.g. Huntington's chorea, drug-induced psychosis). Assessment includes family, psychological and social assessments and corroborative histories.
Initial Service Options Cases can be managed in the community with sufficient outpatient resources such as a clinic, day hospital, and Community Psychiatric Nurse support. This is possible when the diagnosis is clear-cut and where the illness is 'mild'. In cases where there is loss of insight, refusal of treatment, and perhaps violent behaviour (based on, say, delusions or hallucinations) towards the self or others, then inpatient assessment or treatment is required. If consent to admission is not forthcoming, then depending on the circumstances, use of mental health legislation may be needed. Once a firm diagnosis is made treatment can begin, with a move to maintenance treatment with i.m. depot injections as an option. Inpatient and day hospital stays might be from a few weeks to a year.
Medium-term Service Options
Patients in remission can be managed in the community or with day hospital back-up. Patients may attend a variety of voluntary and state support services designed to rehabilitate them. Such facilities include social service drop-in centres, MIND day centres, and clinics. CPN support and computer follow-up to monitor and give treatment is essential to prevent patients 'falling through the net'.
Long-term service Options
If relapse occurs rapid treatment responses in clinic may prevent a further inpatient stay. Further episodes may require re-admission to the day hospital or inpatient facilities. Once the episode is under control, return to the community can be re-negotiated. Persistent psychosis may require altered treatment strategies, e.g. with clozapine, or admission to dedicated rehabilitation wards. There will always be a need for long-term hospitalisation in a minority of cases.
Some dedicated sheltered housing is sometimes available through voluntary and charitable agencies.
Most cases can be adequately managed in the community, usually in their own homes by liaison between CPNs, GPs, psychiatrists and social services.
Improving the future for schizophrenia
Improving outcomes in schizophrenia will necessarily involve new pharmacological treatments and also implementing psychosocial therapies to reduce relapse rates. The psychiatric care team should not restrict its expectations on the basis of past practice. New treatment, education and resource initiatives may substantially improve the lot of people with schizophrenia and their families.
New pharmacological treatments such as ziprasidone, clozapine, olanzapine , risperidone, zotepine and quetiapine offer at least equivalent efficacy to early traditional antipsychotics such as chlorpromazine and reduced side effect profiles.
The caring professions and other need to work together to reduce the stigmata of the disease - maybe by seeking to inform the media and create a dialogue. Psychiatrists badly need to reverse the erroneous and damaging ideas of the nineteen seventies e.g. that inpatient facilities are not required or that schizophrenia does not exist or even that schizophrenia attributable to parental malpractice (sometimes referred to as the double bind hypothesis).
Psychiatrists need to give thought to improving negative symptoms even though it is difficult to treat cognitive deficits that preceded antipsychotics and preceded first psychosis. Psychiatrist must advocate, where appropriate their patients' rights to new treatments - especially where there is good evidence for a proven reduced rate of relapse, fewer unpleasant side effects, increased efficacy leading to increased insight and increased compliance, reduced tardive dyskinesia (with medicolegal consequences), reduced cognitive slowing. Unfortunately some side effects such as sexual side effects and weight gain are not necessarily improved by the newer antipsychotics e.g. risperidone causing retrograde ejaculation. Cognitive behavioural interventions have been found to improve compliance (measured by informants and observers) by improving information supply to patients ( Kemp, R, et al, 1996) Such psychoeducation is a worthy new step forward in engaging sufferers and carers.
Evidence - Based Treatment?
Acute and long-term antipsychotics:
At least 70% of patients in the acute phase do get better (with 300-750mg Chlorpromazine [CPZ] equivalent)
Relapse prevention reqquires 300-600mg CPZ equivalent
Adjuncts
Carbamazepine and benzodiazepines may have additional antipsychotic effects
Psychological interventions
Dynamic psychotherapies have no evidence to suggest an effect on their behalf. There is evidence of modest effects for skill training and supportive individual and group therapies. There is encouraging early evidence for the efficacy of cognitive behavioural therapy.
Family Treatments
Multi-family psychoeducatoional groups reduce relapses over periods as long as four years when used with medications (e.g. McFarlane, 1995).. Such groups present schizophrenia as an illness, not something caused by family prpocesses and instead use that family as co-therapists. Lam's useful review of empirical studies suggested that itwas most useful to focus on the 'here and now', cognitive re-structuring, and improving family communications
Vocational rehabilitation
Evidence poor for overall improvements. Some use in maintaining vocational skills, but may not generalise to the workplace.
Assertive community treatment (ACT)
24 hour availability - intense programmes, but heterogenity in countries/regions Reduces rate and length of admission May reduce costs, but only by a little if at all. If not continuous patients will relapse/degrade Need to start a dialogue with purchasers about family interventions, and severe underfunding, re-focus on evidence based initiatives.
Self-Assessment
Psychiatric Trainees should read the following problem- based case histories and ask themselves the questions that follow, and where necessary using references at the end to research the answers.
Case History One
Jane was seen by a consultant on a domiciliary visit to the vicarage of St.Mary's church. Her father, the vicar, explained that Jane was a sixth form pupil at a local private school. She had always done well at school and had achieved high grades in her fifth form exams. She was hoping to go to University. Over the last few months though her behaviour had changed. She had started refusing to go to school, but had declined to give any reason why. She spent her days writing in her room, and had not eaten for the last three days. She would not let her parents in to see her and had barricaded the door. There was no history of drug abuse.
The consultant talked to her through the door, and finally persuaded her to trust him sufficiently to let him in to her room. He found that Jane was a tall, thin girl with a pale face. The room smelt of urine, and the walls had been covered in a fine, spidery writing. When the consultant tried to read what it said, she shouted at him. Jane looked at him suspiciously and, at times seemed to be conferring with an unseen person as to how trustworthy the doctor was. The doctor could see scratch marks on her neck where Jane had cut herself with the blade of a pair of scissors. She said that this was 'to let the bad blood out'. Jane appeared alert and knew the day and the time. When asked about her refusal to eat, Jane mumbled about her parents trying to poison her, because, she said, ' my mother offered me an Arrowroot Thin biscuit...that would make me thin...and she offered me some cabbage...that would turn me into a cabbage.'
The doctor felt that Jane's health was at risk because she had been harming and starving herself, and that there was evidence of a mental disorder which warranted admission to hospital for further assessment.
What evidence is there that Jane is suffering from a psychotic disorder?
What evidence suggest that this is not an acute organic psychosis?
What are the diagnostic features of schizophrenia in this case?
Why does schizophrenia often appear to begin in adolescence?
Case History Two.
J. Albert Arthur Andrew Churchill Chamberlain was a man who went under several aliases and had a career as a small time con-man. Some days he was Albert Chamberlain and some days he was Andrew Churchill.
He presented to his general practitioner with feelings of 'great sadness and loss of sincerity'', as he put it. His general practitioner found his speech difficult to understand, but his main concerns seemed to be about his ex-wife. He claimed that his ex-wife was plotting with the British Security Forces to remove his 'sincerity and personality'. The GP noted down some of his speech verbatim: "My divorced wife has an albigisty of conscience which she has terpolated with the Security Forces. They're debating my existence even now. They're saying we will drain his face of emotions, put our emotions into him and alter what the doctor's writing on the page to alter the circumstance and the circumcision of the truth."
On further questioning the patient seemed wholly convinced that a transmitter had been inserted into his neck - he said he could actually feel it there - and that the transmitter was designed to put his wife's thoughts into his head. He could distinctly hear conversations between his wife and agents of the British security Forces commenting on his thoughts and actions.
What Schneiderian first rank features does this patient exhibit?
What is the significance of his using words like 'albigisty' and 'terpolated'?
What kind of schizophrenia is this?
Case History Three.
Shakil, 32, was brought to casualty by his brother. His brother had found him in a nearby seaside town, by accident. Shakil had been missing from home for several years. By chance his brother had seen Shakil walking down the road and had followed him home. Home had turned out to be ramshackle flat above an empty sewing machine shop. His brother had been disgusted to find the remains of Shakil's last meal, an unplucked, ungutted and uncooked pigeon. Shakil said he had put the bird in the oven for half-an-hour to cook it, but since the electricity supply had been long since discontinued, the attempt had been pointless. Shakil had been unwilling to draw unemployment benefit, because he said the money should be sent to the third world instead. A god, called Abu-Lafram, living in the bathroom, had told Shakil that he should deny himself for the benefit of the third world. Shakil had little furniture left - he had sold most of it to buy bread and aluminium tin foil. He had used the tin foil to line the walls of the flat, to protect Abu Lafram from the evils of Western civilisation that seeped through the walls. His brother had been most upset when he had told Shakil the bad news that his mother had died whilst Shakil had been away from home. Shakil had started to laugh.
On interview in casualty Shakil was unkempt and dressed in a grimy boiler suit, to which adhered blood and feathers. A large pentagram was daubed on the breast pocket. Shakil giggled at times and appeared to be listening to some voice that other people could not hear. He was mildly thought disordered and distractible, pacing about casualty, preaching the gospel of Abu-Lafram to other patients, using various neologisms. When he was asked how he felt about the death of his mother, Shakil grinned and said that his mother was a 'white cloud in a darkening and prejudiced sky'.
He claimed to be a prophet of Abu-Lafram, and that he had been chosen as his first earthly disciple. Abu-Lafram talked to him throughout the day in a sonorous male voice, 'realer than the realest reality'. The thoughts he had had since knowing Abu-Lafram were 'the purest of pure'' and were broadcast out of Shakil's head by Abu-Lafram for 'the benefit of all mankind'. Shakil did not believe that he was ill, but was adamant that he was a 'chosen one'.
What evidence is there to support a diagnosis of schizophrenia? What is the relevance of the patient's lack of insight?
Further Reading and References
Texts
Andrews & Jenkins (Editors) (2000) Management of Mental Disorders. Volume 2. World Health Organisation
Gelder, M, Gath, D & Mayou, R. (1989 ) Oxford Textbook of Psychiatry, (Chapter 9. Schizophrenia and schizophrenia-like disorders,. pp. 268-323). Oxford, Oxford Medical Publications.
Kendell, RE, & Zealley, AK. (1993) Companion to Psychiatric Studies. 5th edition. (Chapter 18. Schizophrenia. pp. 397-426).Edinburgh, Churchill Livingstone.
Sims, A. (1988) Symptoms in the Mind. (Chapter 8. Disorders of the thinking process. pp. 105-125) Oxford, Bailiere Tindall.
Papers
Andreasen, N (1990) Magnetic resonance imaging of the brain in schizophrenia. Arch. Gen.Psychiatry, 47, 35-44.
Jones, P et al (1994) Child development risk factors for adult schizophenia in the British 1946 birth cohort. Lancet, 344, 1398-402.
Kemp, R, et al. (1996) Compliance therapy in psychotic patients: randomised controlled trial, BMJ 312, 345-9
Lam D H (1991) Psychosocial family intervention in schizophrenia: a review of empirical studies. Psychological Medicine, 21, 423-441
McFarlane, W R et al (1995) Psychoeducational multiple family groups: four year relapse outcome in schizophrenia. Fam. Process, 34, 127-44.
McNeil, TF, Harty, B, Bennow, G et al. (1993) Neuromotor deviation in offspring of psychotic mothers: a selective developmental deficiency in two groups of children at heightened psychiatric risk? J. Psychiatric Research, 27 (21), 39-54.
Murray, RM, Jones, P, O' Callaghan, E et al. (1992) Genes, viruses and neurodevelopmental schizophrenia. J Psychiatric Research. 26 (4), 225-35.
Shepherd, M, Watt, D, Falloon, I, et al. (1989) The natural history of schizophrenia: a five-year follow-up study of outcome and prediction in a representative sample of schizophrenics. Psychological Medicine, (Suppl. 15), 46.
Timms, P W. & Fry, A H (1989) Homelessness and mental health. Health Trends, 21, 70-71.
Tsuang, MT, Woolson, RF, Fleming, JA. (1979) Long-term outcome of major psychoses. Arch. Gen. Psychiatry, 36, 1295.
Vaughn, CE, & Leff, JP. (1976) Influence of family and social factors on the course of psychiatric illness. B J Psych, 129, 125.
Copyright © Priory Lodge Education Limited 2007
Click
on these links to visit our Journals:
Psychiatry
On-Line
Dentistry On-Line | Vet
On-Line | Chest Medicine
On-Line
GP
On-Line | Pharmacy
On-Line | Anaesthesia
On-Line | Medicine
On-Line
Family Medical
Practice On-Line
Home • Journals • Search • Rules for Authors • Submit a Paper • Sponsor us
All pages in this site copyright ©Priory Lodge Education Ltd 1994-


