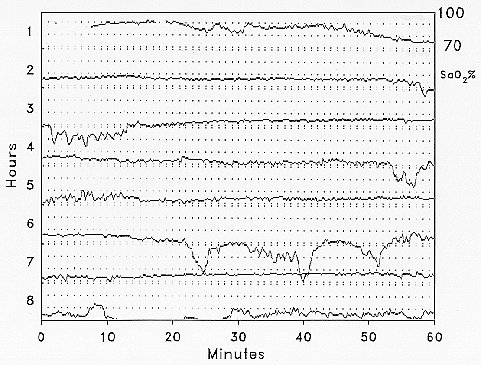
There can be large falls in arterial oxygen saturation during sleep in patients with chronic obstructive pulmonary disease. In general, these falls can be predicted from daytime oxygen levels and are not due to classical OSA syndrome, but to a number of factors which combine to produce worsening hypoxaemia during sleep. These patients are often at the limits of their respiratory capacity, and the loss of the intercostal and accessory muscle contribution to breathing, and the increase in upper airways resistance associated with REM sleep, cause marked falls in ventilation. In addition, patients may be hypoxic while awake and small falls in ventilation and PaO2 lead to large falls in arterial oxygen saturation during sleep. The hypoxic episodes demonstrated by overnight oximetry in a patient with chronic obstructive pulmonary disease differ in character from those seen in patients with OSA syndrome (figure 10).
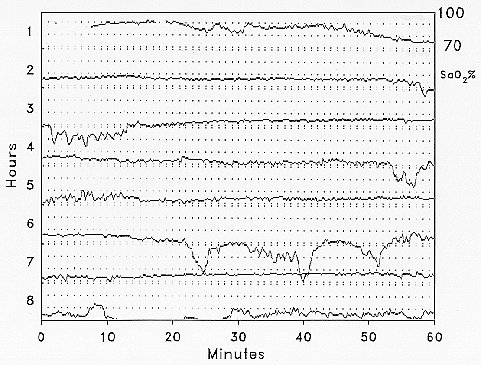
Figure 10. Overnight arterial oxygen saturation monitoring in a patient with chronic obstructive pulmonary disease.
There is some evidence that increases in upper airway narrowing during sleep, short of apnoeas and even snoring, may contribute to the development of CO2 retention in these patients. However classical sleep apnoea is not significantly more common in unselected COPD patients with raised CO2 levels, and excessive nocturnal hypoxaemia is not one of the predictors of long- term survival in patients with COPD.