The traditional definition of sleep apnoea, that is apnoea of 10 seconds or longer occurring five or more times per hour of sleep, failed to appreciate the true nature of this condition. It was unnecessarily restrictive and failed to take account of the two linked events that are central to the development of daytime symptoms in these patients. These are:-
Although obstructive apnoeas of more than 10 seconds do result from excessive upper airway narrowing and lead to arousals, they are not the only events to do so. The upper airway narrowing in normal subjects referred to earlier is usually of no consequence, because the slight increase in inspiratory effort that results does not lead to arousal. Once the increased upper airway narrowing leads to sufficiently increased inspiratory effort to provoke arousal, then there is the potential for daytime symptoms to develop due to recurrent sleep fragmentation.
We now know that even snoring alone (without apnoeas, hypopnoeas, or hypoxia) can provoke recurrent arousals and daytime symptoms indistinguishable from the classic presentation with full apnoeas. Furthermore, the relationship between nocturnal events and daytime symptoms is very limited, making arbitrary definitions of abnormality based on sleep studies impossible. Thus rigid definitions of normality versus abnormality are currently impossible in this area, and one is forced to use clinical definitions for the disorder: for example, significant daytime symptoms (sleepiness etc., see later) in conjunction with evidence of sleep related upper airway obstruction (snoring, hypopnoeas, apnoeas) and sleep disturbance (EEG arousals, body movements, autonomic activation etc.). Such definitions have important consequences when designing sleep studies and deciding upon treatment (see later).
OSA syndrome is the most common cause of sleep-disordered breathing. Community surveys indicate that the condition may be symptomatic in up to 1% of apparently normal men of working age. There is wide variation in the severity of OSA from short periods of recurrent sleep disruption with snoring, which are present in over 5% of asymptomatic men, to the full classical syndrome in which the patient can never sleep and breathe at the same time.
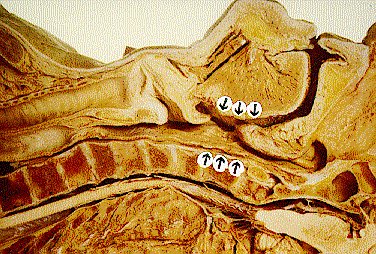
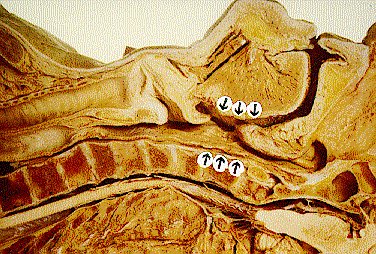
Figure 1. Anatomy of
obstructive sleep apnoea.
Coronal section of the head and neck showing
the segment over which sleep related narrowing can occur
(arrows).
The critical event in obstructive sleep apnoea and it's variants is the narrowing and collapse of the pharyngeal airway with the onset of sleep (figure 1). This can occur anywhere along it's length, from the soft palate to just above the epiglottis. The collapse can be complete (apnoea) or partial (when snoring is usually present) and leads to increased inspiratory efforts, sometimes to pleural pressures of -80 cms H2O or so. After a variable period (from a few seconds to over 2 minutes), arousal occurs with the opening of the airway and, almost always, loud snoring. The derangement of blood gases that usually develops during an apnoea or hypopnoea is then rapidly corrected by a short period of hyperventilation.
The arousal mechanism is probably multifactorial, but pharyngeal and/or pleural receptors sensing the increased inspiratory effort are probably the most important. The deterioration in blood gases (asphyxia) is likely to be contributory since this is clearly the arousal stimulus in central apnoeas when no inspiratory efforts are made. It is the arousal and the consequent increase in pharyngeal muscular tone that pulls the airway open, ends the period of obstruction, and allows the resumption of ventilation. After a short period, sleep resumes and the cycle is repeated.
A patient with severe sleep apnoea can experience 300 - 500 of these events in one night, with sleep occurring in short intervals no longer than the longest period of apnoea (usually less than 60s). With such a severe disturbance to sleep architecture, the deeper refreshing stages of sleep (i.e. SWS) are seldom entered, and it is easy to see why these patients are hypersomnolent.
The severity of sleep apnoea, as judged by conventional definitions (numbers of apnoeas, distribution of sleep states etc.), correlates poorly with daytime symptoms. It is likely that the degree of arousal from sleep, the length of any interapnoeic periods, as well as the number of arousals, are the important factors in determining the symptom of hypersomnolence.
Pharyngeal airway: the pharynx has to serve two very different functions - breathing and eating. When air is the only consideration, the trachea can be a rigid incompressible tube; when food and drink are the only consideration, the oesophagus can be a floppy muscular tube propelling material along it's lumen. The pharynx accomplishes both functions by having a complicated set of muscles that can hold it open during breathing, but when relaxed allow the propulsion of food and drink by peristalsis.
The factors that oppose these muscular dilator forces are intrapharyngeal negative pressure, intrapharyngeal space occupying masses, and external compression. During inspiration, there is a subatmospheric pressure in the pharyngeal lumen due to the normal upstream resistance in the nose; if there is a high nasal resistance, the pressure difference will be even greater. During normal breathing, increases in phasic inspiratory pharyngeal muscular tone combat this increased suction. External compression (e.g. mass loading by fat) also tends to cause closure against which the pharyngeal muscles must act.
Another important factor affecting the balance of forces in the pharynx is the starting size of the lumen. If the lumen is encroached on by, for example, tonsillar hypertrophy, or abnormal tissue deposition (e.g. in acromegaly, hypothyroidism and the mucopolysaccharidoses), then it is easier for the lumen to be further obliterated. Other important provoking anatomical factors are the dimensions of the lower face. Quite subtle degrees of underdevelopment and retropositioning of the mandible and maxilla contribute to the development of sleep apnoea. This particular facial shape may to some extent be hereditary, although there is also evidence that prolonged mouth breathing as an infant can produce similar changes (sometimes called the adenoidal facies).
The main risk factor for obstructive sleep apnoea is obesity. Quite how obesity produces sleep apnoea is not clear, but recent evidence has suggested that simple mass loading of the neck overcomes the ability of the pharyngeal muscles to maintain a lumen during sleep, when the tonic postural input to these muscles is withdrawn. Studies have shown that the tendency to have sleep apnoea correlates better with neck circumference than with general obesity, and that a neck circumference of more than 43 cm (17 inches) is the most significant predictor of the presence of OSA syndrome.
A unifying concept drawing all this together is that excess weight in the neck loads the pharyngeal dilators even when the patient is awake, but that the increased muscular activity due to tonic postural input is effective in maintaining a lumen. With the onset of sleep, this compensation may be lost thus allowing the external weight to compromise the airway, particularly in the presence of prior structural narrowing from a degree of retrognathia or tonsillar hypertrophy.
Sedative drugs, such as alcohol and the benzodiazepines, reduce muscular tone in the pharynx and can produce snoring or provoke obstructive apnoeas in snorers. Thus, it is important to enquire about alcohol and sedative use in patients with suspected sleep apnoea.
OSA syndrome is being increasingly recognised in children and is mainly caused by tonsillar enlargement (occasionally only minimal). In many of these children there is no apnoea at all and it is snoring alone that produces the symptoms. Tonsillectomy virtually always leads to rapid relief of symptoms, which are often less specific than in adults: they include hyperactivity, bad behaviour, poor school performance and enuresis, as well as the loud snoring. Because tonsillar size fluctuates in children (due to upper respiratory infections), the snoring and symptoms will fluctuate and a one-off sleep study may be deceptively normal. Thus the parents' history may be more indicative of a significant problem than the sleep study.