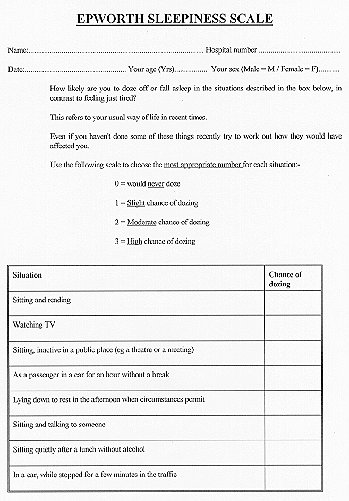
Hypersomnolence in patients with OSA syndrome can be profound with the onset of irresistible sleep during talking, driving and eating. As the condition worsens, progressively more and more stimulation is required to maintain arousal. In the early stages, the hypersomnolence may be noticeable only during boring activities. Car accidents are more common in sleep apnoea sufferers, but concerns about losing one's driving licence lead to under -reporting of drowsiness while driving. The Epworth sleepiness score is a simple verified way to document the degree of sleepiness although occasionally it fails to represent the degree of sleepiness (figure 3).
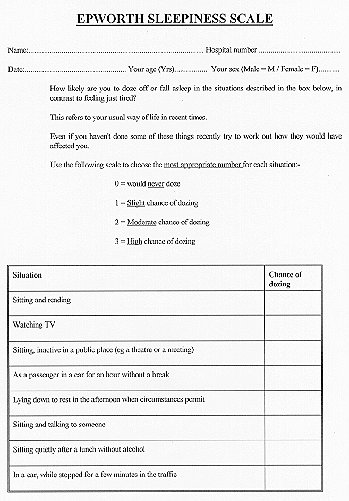
Figure 3. Assessment of
sleepiness using the Epworth sleepiness scale.
This questionnaire can be filled in by the
patient unattended.
A total score up to about 9 is considered normal and most
patients with severe OSA syndrome will be above 15.
Snoring: the prevalence of regular snoring increases with age and is more common in men than women; approximately 25% of men and 5-10% of women aged 35-65 years snore. Recent population surveys have found a strong correlation between snoring and daytime sleepiness, which probably results from the sleep disturbance that snoring alone can produce, without necessarily any sleep apnoea, as discussed earlier. At an epidemiological level there are probably more people with excessive daytime sleepiness due to snoring that from classical OSA syndrome with full apnoeas. However, in most sleep clinics, reporting of apnoeas by the bed partner has been more predictive, than just snoring alone, of actual sleep apnoea on a subsequent sleep study.
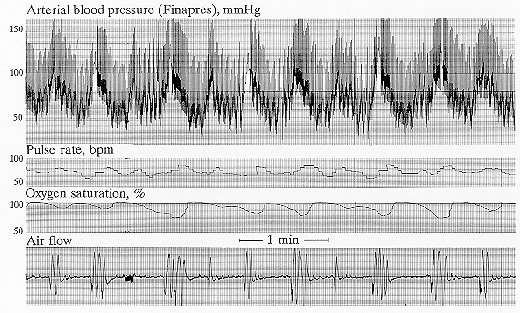
Figure 4. Non-invasive
monitoring of systemic blood pressure in a patient with
obstructive sleep apnoea.
During an apnoea (no air flow) the obstructed inspiratory
efforts lead to falls in pleural pressure that are reflected in
the blood pressure tracing. At the end of an apnoea the arousal
provokes a rise in blood pressure.
One of the most dramatic physiological consequences of OSA is the large rise in systemic blood pressure that occurs at the end of each apnoeic episode (figure 4). Systolic blood pressure can increase by up to 100 mmHg, 300-400 times each night in severe cases. It had been thought that hypoxaemia played a central role in the development of these blood pressure swings, but recent evidence shows that arousal from sleep is sufficient to cause the rise in blood pressure. Although there is no definitive evidence that these blood pressure swings have deleterious long term effects, intuitively it does seem likely. It has been suggested that normal sleep enhances longevity by reducing cardiovascular workload (i.e. fall in blood pressure, heart rate and vascular resistance) and that these recurrent periods of hypertension may well be harmful. This view is supported by some evidence of increased cardiovascular mortality in patients with OSA. Most of the available studies do not have ideal controls and a large retrospective survey of sleep clinic patients did not find the presence of OSA to be an independent risk factor for cardiovascular death.
A direct cause and effect relationship between sleep apnoea and sustained daytime hypertension now looks increasingly doubtful. Recent large studies have found that the occurrence of OSA syndrome and hypertension together is almost entirely due to an important common risk factor - obesity. However early morning, post-sleep, blood pressures may be independently affected by the presence of sleep apnoeas.
Although in early reports cor pulmonale was fairly common in patients with obstructive sleep apnoea, it is now clear that these patients were at the severe end of the disease spectrum. Patients are now being recognised earlier and associated cor pulmonale is a much less common finding. It is also clear that another factor, in addition to obstructive sleep apnoea, probably needs to be present to provoke diurnal respiratory failure and fluid retention. This is usually either a degree of lower airways obstruction (e.g. from smoking), gross obesity or respiratory muscle weakness. However, the lower airways obstruction need only be mild, and hypercapnia out of proportion to the degree of lung disease and breathlessness should suggest OSA syndrome as a possible additional diagnosis, particularly in the presence of other symptoms such as snoring and sleepiness.
The diagnosis is often made on the history alone. The probability of obstructive sleep apnoea in a sleepy patient with a large neck, and a long history of loud snoring, witnessed apnoeas, and restless sleep is extremely high. However, some form of confirmatory study is considered essential before starting treatment.
Visual observation of sleep: the frustrated, struggling inspiration, often for over 1 minute, followed by noisy resumption of breathing with variable arousals, is easily recognised once seen. It is important to observe sleep in both the supine and decubitus postures, as obstruction occurring in the supine posture can be simply relieved by position training. Failure to observe apnoeas during a short period of sleep does not of course exclude OSA syndrome.
Pulse oximetry is another simple screening method and also provides a continuous reading of heart rate (a marker of arousal). Modern equipment enables the arterial oxygen saturation and pulse rate to be recorded for at least 8 hours overnight and can be used at home.
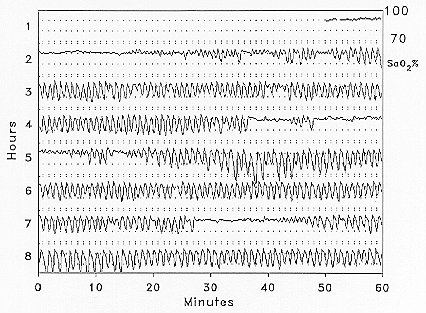
Figure 5a. Overnight arterial
oxygen saturation monitoring.
A patient with severe obstructive sleep apnoea. Recording
shows multiple dips in oxygen saturation.
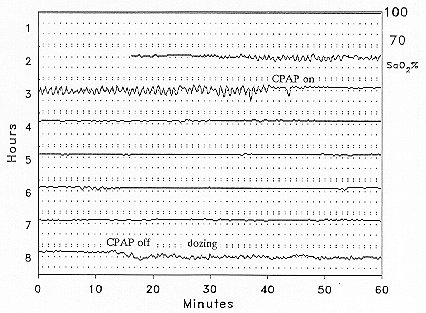
Figure 5b. Overnight arterial
oxygen saturation monitoring.
The same patient while receiving continuous positive airway
pressure via a nasal mask throughout the night.
The recording shows the abolition of dips and is essentially a
normal tracing.
Figure 5a shows a recording of the SaO2 characteristic of OSA syndrome. A totally flat trace in a patient who says he slept well virtually excludes the diagnosis. Results between these two extremes may require more extensive studies, particularly if recurrent arousals due to heavy snoring alone are to be recognised.
Oximetry and video: the addition of an all-night video recording is useful, as doubtful areas on the oximetry trace can be reviewed to confirm if any sleep and breathing disorder is present. A further development of oximetry and video recordings has been to process the video signal digitally to detect body movements as another marker of arousals in addition to rises in heart rate (See Stowood Scientific Instruments). Tracings of movement, SaO2, pulse rate and snoring are very characteristic in classic OSA, snoring with arousals and snoring alone; if all four tracings are flat then a sleep and breathing disorder is excluded (figure 6).
Figure 6. Overnight monitoring using oximetry and video recordings.
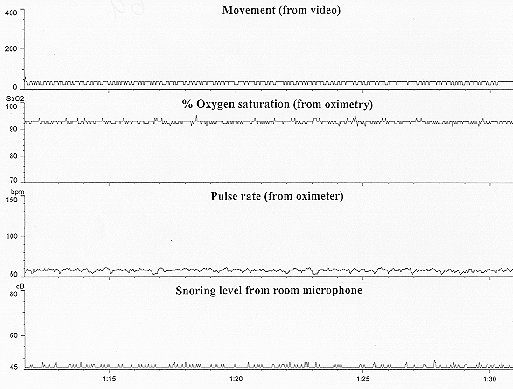
Figure 6a.
The four tracings represent body movement (processed from the
video signal), oxygen saturation, pulse rate and noise/snoring
volume (in dB, where 45 dB is background levels and 55dB is quiet
snoring). This is a normal tracing with four flat lines
throughout with no evidence of snoring, hypoxaemia or recurrent
arousals.
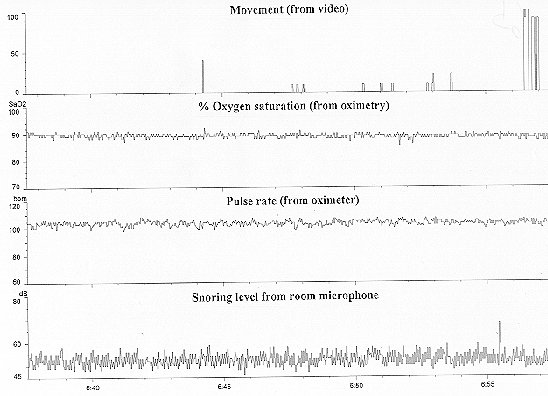
Figure 6b.
A patient with continuous snoring but no evidence of multiple
arousals in that the pulse rate is steady and there are very few
body movements. In addition there are no dips in oxygen
saturation.
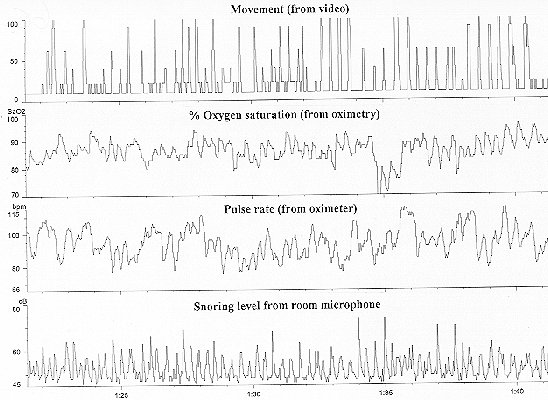
Figure 6c.
This patient with OSA shows the typical snore/silence/snore
pattern in association with body movements and pulse rate rises
indicating sleep disturbance, and falls in oxygen saturation
showing that the obstruction has been bad enough to interfere
with gas exchange.
Such simple sleep study techniques have always been compared with full polysomnography. However this is incorrect. Full polysomnography missed the partial forms of sleep apnoea (snoring induced arousals for example) and is not a good gold standard. The correct way to evaluate sleep monitoring equipment is to assess its ability to recognise those patients with a sleep related upper airways problem that will respond to definitive treatment. In future, response to treatment (such as nasal CPAP, see later) is likely to be the gold standard against which the success of diagnostic tests is judged.
Full polysomnography, in which many physiological variables are monitored, used to be regarded as the gold standard. It may include:
Despite the availability of sophisticated automated analysis and reporting systems, the interpretation of all these different physiological signals requires considerable experience, not least because of the numerous artefacts produced during sleep recordings.