
Treatment must be tailored to the individual patient's symptoms. The main driving force to treat is the hypersomnolence or other daytime symptoms, not the sleep study 'severity'. In mild OSA, simple therapeutic measures, such as avoidance of alcohol or sedatives (which further suppress upper airway tone), weight loss (particularly successful if lost from around the neck), mandibular advancement devices and reduction of nasal resistance, often suffice. In a few patients, in whom obstructive sleep apnoea only occurs when they lie supine, measures to maintain sleep when lying flat may be successful. Clearly, any underlying cause, such as hypothyroidism or acromegaly, must be sought and treated.
Continuous positive airway pressure therapy (CPAP): in severe cases with disabling symptoms, it is necessary to provide CPAP from a fan pump, delivered via a nasal mask (figure 7).

Figure 7. CPAP nasal mask.
Nasal mask used for continuous positive airway pressure. The same type of mask can be
used for nasal ventilation.
This provides a "pneumatic" splint that literally blows open the pharynx to allow unobstructed breathing, with striking results on pulse oximetry (figure 5b) and abolition of the blood pressure swings. The resolution of the disabling symptoms can be dramatic and explains why such cumbersome and unaesthetic equipment is well tolerated, (figure 8).
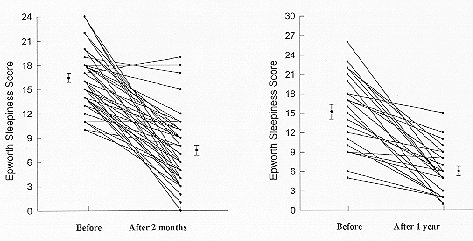
Figure 8. Resolution of sleepiness after
nasal CPAP therapy.
Epworth sleepiness scores (see figure 3) before and after a period on nasal CPAP. Most
patients are within the normal range following treatment.
Manual titration of the individual pressure required by the patient overnight used to be required, now this process can be done quite adequately automatically by so-called 'intelligent' CPAP machines. These sense snoring, flow limitation, hypopnoeas and apnoeas which leads to appropriate raising or lowering of the pressure. This overnight pressure profile can then be reviewed in the morning and an appropriate fixed pressure chosen for subsequent home use. There is no evidence that use of an 'intelligent' machine is of any value used at home long-term, although there are theoretical reasons why it might be.
Mandibular advancement devices: Moving the jaw forward enlarges the retroglossal airspace. This can be achieved during sleep by the used of an intraoral device that fixes to upper and lower teeth. The simplest form of such devices consists of a pair of custom made gum shields for the top and bottom teeth that are welded together with the lower jaw held closed and protruded forward by about 75% of maximum protrusion, figure 9.
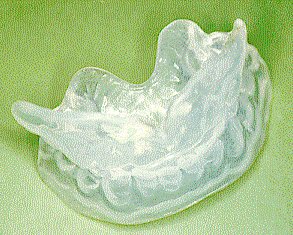
Figure 9. Mandibular advancement device.
Simple oral appliance constructed from two custom made gum shields. Worn at night this
increases the retroglossal space and reduces upper airway resistance.
There is good evidence that this approach works for snoring and mild-to-moderate OSA, but there are some problems with tolerability (though probably less than with CPAP).
Surgery: the clear indication for surgery is the removal of enlarged tonsils or other obstructing "tumours". The operation of uvulopalatopharyngoplasty (removal and reshaping of the soft palate and pharynx) has dropped out of favour for the treatment of OSA although it clearly can work in some carefully selected cases. We regard it as second or third line treatment when other, non-destructive, approaches have failed, i.e. CPAP (with humidifier if necessary) or dental appliance. It may still be an appropriate treatment for loud snoring in carefully selected cases, although objective evidence suggests that the benefits are very small compared to the subjective reports.